Cataracts are a medical condition in which the lens inside the eye becomes progressively opaque, leading to blurred vision and blindness if left untreated (Fang et al., 2022). Cataracts are the leading cause of blindness worldwide, affecting around 65 million people. The prevalence of cataracts increases with age, ranging from around 4% in people aged 55-59 to over 90% in people aged 80 and above (The clinical effectiveness and cost, n.d.). As the global population ages, cataracts are becoming an increasingly important public health issue.
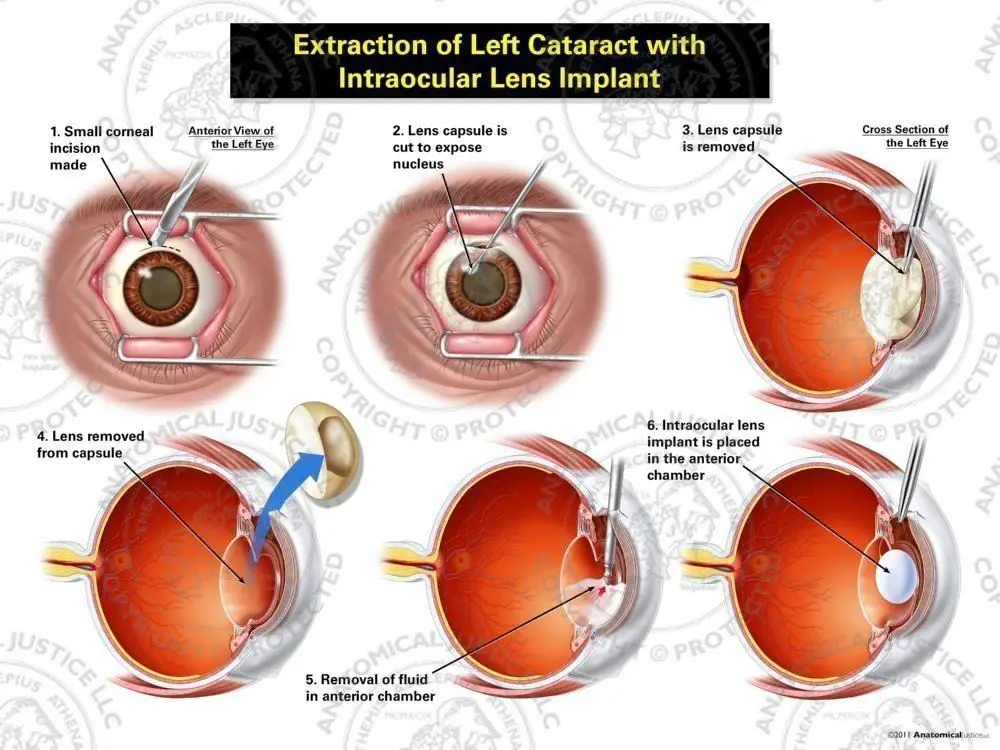
Cataract surgery is the only effective treatment for cataracts. During cataract surgery, the cloudy natural lens is removed and replaced with an artificial intraocular lens implant. The surgery aims to restore vision by making the lens clear again. There are several different techniques and procedures for cataract surgery, each with their own potential benefits and drawbacks. The three main types of cataract surgery are phacoemulsification, extracapsular cataract extraction, and intracapsular cataract extraction.
Phacoemulsification
Phacoemulsification is the most common and preferred method of cataract surgery today (Source). It uses ultrasonic energy to break up the cloudy lens, or cataract, and remove the pieces from the eye.
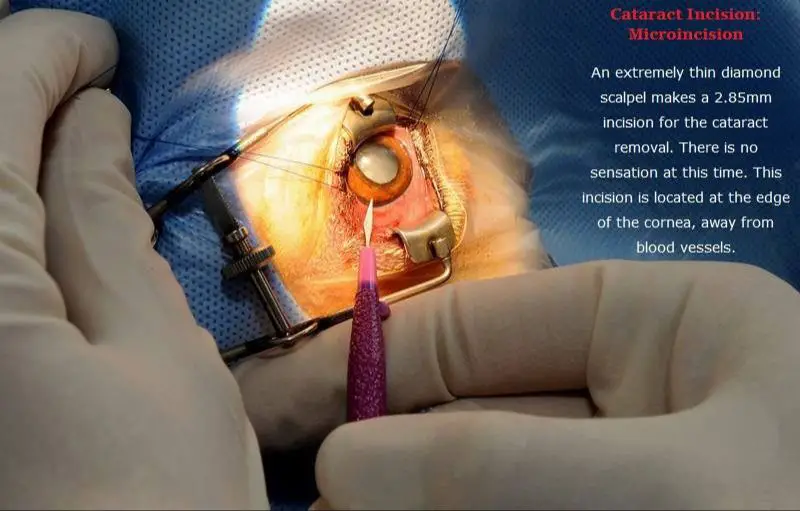
During phacoemulsification, the surgeon makes a tiny incision in the cornea. A small probe is inserted into the eye and emits ultrasonic waves that soften and break up the cataract. The pieces are then suctioned out. Typically, an artificial intraocular lens (IOL) is implanted in the same procedure to replace the natural lens and restore vision.
The main benefits of phacoemulsification include:
- Smaller incision size than other cataract procedures
- Faster healing time
- Less post-operative astigmatism
- Lower risk of complications
- Improved visual outcomes
Phacoemulsification generally has faster recovery times and better visual acuity results compared to other cataract surgery techniques. Most ophthalmologists perform phacoemulsification for cataract removal today.
Extracapsular Cataract Extraction
Extracapsular cataract extraction (ECCE) is a type of cataract surgery where the lens nucleus and inner cortex are removed in one piece through a 10-12mm incision, leaving the posterior capsule intact (Source). The main steps involve making the incision, extracting the nucleus and cortex, and inserting an artificial intraocular lens (IOL) into the empty capsule.

The key benefit of ECCE is preserving the integrity of the posterior capsule, which provides support for the IOL and helps maintain the vitreous body. This tends to result in better postoperative visual outcomes compared to intracapsular cataract extraction. ECCE also lowers the risk of retinal detachment and cystoid macular edema. However, the larger incision increases recovery time and the risk of post-op astigmatism compared to modern small-incision phacoemulsification.
Intracapsular Cataract Extraction
Intracapsular cataract extraction (ICCE) is a type of cataract surgery where the entire natural lens and surrounding lens capsule are removed in one piece through a large incision in the cornea or sclera (white part of the eye) [1]. This was one of the earliest surgical techniques for cataract removal, but has become less common with the development of smaller-incision extracapsular techniques.
In ICCE, the surgeon makes an incision of 10-12 mm and removes the central portion of the anterior capsule along with the lens nucleus and cortex [2]. The intact posterior capsule is left within the eye. A large incision is necessary because the entire lens is removed intact. After surgery, thick glasses or contact lenses are required to regain vision [1].
Benefits of ICCE include complete removal of the cataractous lens, which reduces the risk of posterior capsule opacification. It may be preferred in cases of hypermature or intumescent cataracts that have liquefied or leaked lens material into the eye [2]. However, the large incision increases recovery time and the risk of postoperative astigmatism, infection, and retinal detachment.
[1] https://www.sciencedirect.com/topics/nursing-and-health-professions/intracapsular-cataract-extraction
[2] https://www.ncbi.nlm.nih.gov/books/NBK559253/
Choosing a Procedure
There are several factors to consider when choosing the right cataract surgery procedure, including cost, recovery time, and potential complications.
Phacoemulsification is the most common and preferred procedure in developed countries, accounting for approximately 90% of cataract surgeries performed. It has a lower complication rate compared to extracapsular surgery and involves a smaller incision, allowing for faster healing and visual recovery. According to research, phacoemulsification may have slightly higher costs but lower overall healthcare utilization costs compared to extracapsular surgery due to the faster recovery time (https://pubmed.ncbi.nlm.nih.gov/24366765/).
Extracapsular surgery is more affordable but involves a larger incision and longer recovery time. There is also a higher risk of complications such as retinal detachment. However, it may be preferable in patients with very dense cataracts or weak zonular support. Recovery can take 4-6 weeks before vision stabilizes.
Intracapsular surgery has largely been replaced by extracapsular techniques due to higher complication rates. It requires removal of the entire lens capsule and lens matter, resulting in greater surgical trauma. However, it may still be performed in rare cases of severe zonular weakness.
The ophthalmologist will determine the best procedure based on the type and severity of the cataract, eye anatomy, and the patient’s overall health. Less invasive phacoemulsification is preferable when possible for quicker recovery of vision. However, extracapsular surgery remains an important option for complex cataract cases.
Preparing for Surgery
There are several things you’ll need to do to prepare for cataract surgery. First, your ophthalmologist will perform preoperative tests to determine your eye health and prepare for the procedure. These may include eye measurements, imaging scans, and blood tests (https://www.heartoftexaseye.com/blog/preparing-for-cataract-surgery/).
You will also need to make arrangements for transportation home after surgery, as you cannot drive yourself. It’s recommended to have someone stay with you at least the first night to assist you. In terms of restrictions, you will need to stop taking certain medications ahead of surgery, such as blood thinners, anti-inflammatory drugs, and aspirin. Your doctor will advise you on any medications to avoid. You will also need to fast after midnight the night before surgery.
On the day of surgery, you should avoid wearing makeup, lotions, creams, or fragrances. Wear comfortable clothing and shoes to the surgical center (https://www.silkvision.net/blog/how-prepare-cataract-surgery-8-step-guide). Your eye doctor will provide specific instructions to follow to prepare for the procedure.
During Surgery
The cataract surgery procedure typically follows these main steps:
- The surgeon makes a tiny incision in the cornea to access the lens. This is usually less than 3 mm long.
- The surgeon inserts a special needle into the eye and uses ultrasound waves to break up the cloudy lens into small pieces. This process is called phacoemulsification. (1)
- The broken pieces of the cataract are gently suctioned out of the eye.
- For people having standard cataract surgery, the surgeon places a clear artificial lens called an intraocular lens (IOL) into the empty lens capsule.
- For toric IOLs that correct astigmatism, the surgeon ensures the lens is properly aligned before securing it in place.
- The surgeon uses tiny stitches or self-sealing methods to close the microscopic incision.

The procedure is performed with a high-powered microscope and microsurgical instruments. Patients are usually awake during surgery, but they are given local anesthesia to prevent discomfort. Surgery typically takes less than 30 minutes. Most people do not feel any pain during the procedure.
Recovery
The recovery period after cataract surgery typically lasts around 4-8 weeks (King Edward VII’s Hospital, 2022). Your eye will need time to heal completely. You may experience some temporary side effects like irritation, swelling, redness, sensitivity to light, sticky eyelids, watery eyes, and mild pain or discomfort (NHS, 2022). These side effects usually improve within the first few days, but it can take 4 to 6 weeks for your vision to fully stabilize and adjust.
Your doctor will prescribe eyedrops to prevent infection, reduce inflammation, and help your eye heal properly after surgery. It’s important to use the drops as directed. You may need to wear an eye shield at night to protect your eye while sleeping. Your doctor may also recommend wearing sunglasses outside to minimize light sensitivity.
There are some restrictions after surgery as your eye heals. Your doctor will likely recommend avoiding strenuous activity, bending over, heavy lifting, and rubbing your eye. Do not get water in your operated eye for at least 2 weeks. Avoid driving until your doctor says it’s safe to do so, typically 1-2 weeks. Follow your doctor’s specific advice on activity restrictions.
Results
After cataract surgery, vision typically starts improving within a few days but may be blurry at first as the eye heals [1]. Most patients experience significant improvement in their vision, with many achieving 20/25 vision or better. However, final visual results can take several weeks or months as the eye adjusts [2].
While cataract surgery aims to reduce dependency on glasses, some patients still need glasses for certain activities after surgery. The type of intraocular lens implant chosen affects the need for glasses. Monofocal lenses only correct either near or distance vision, so glasses are still needed for the other range. Multifocal or accommodating lenses aim to reduce reliance on glasses but do not eliminate it entirely.
In most cases, the visual improvements after cataract surgery last for life. However, a small percentage of patients develop clouding of the posterior lens capsule months or years later, which can diminish vision gains. This posterior capsule opacification is treatable with an outpatient laser procedure.
Conclusion
Cataract surgery is an important treatment for restoring vision obscured by cataracts. The three main techniques – phacoemulsification, extracapsular cataract extraction, and intracapsular cataract extraction – each offer advantages and drawbacks. Phacoemulsification, which uses ultrasound to break up and remove the cloudy lens through a small incision, is the most common and advanced procedure today. Extracapsular extraction removes the cloudy core of the lens but leaves some of the capsule intact. Intracapsular extraction removes the entire lens and capsule at once.
While the techniques vary, the goal remains the same – to remove the opacity preventing light from reaching the retina, and replace the natural lens with an artificial intraocular lens implant. With cataract surgery, most patients can regain clear vision, though they will still likely need glasses or contacts for some tasks post-surgery. Thanks to continuing advances in the field, cataract treatment offers safe and effective means for restoring sight.