What are cataracts?
Cataracts are a clouding of the natural lens in the eye that affects vision. The lens is normally clear and helps focus light onto the retina at the back of the eye, allowing you to see clearly. With cataracts, the proteins that make up the lens start to clump together and cause the lens to become cloudy or opaque (Source 1).
As cataracts develop, less light passes through the lens which leads to blurry, hazy, or distorted vision. Colors may start to look faded or yellowish. Night vision and glare tolerance can also be affected. Cataracts typically develop slowly over many years. In the early stages, stronger glasses, anti-glare sunglasses, or brighter lighting may help compensate for vision changes. Over time, as the cataract worsens, these solutions are no longer effective (Source 2).
The most common causes of cataracts are aging and ultraviolet radiation exposure. Other risk factors include diabetes, smoking, excessive alcohol use, certain medications, eye injuries, and family history. Cataracts are extremely common, affecting around 50% of people by age 80 according to the National Eye Institute.
Symptoms of cataracts include:
- Blurry, cloudy, or filmy vision
- Increased sensitivity to light and glare
- Faded or yellowed colors
- Halos or double vision
- Frequent changes in eyeglass or contact lens prescriptions
How cataract surgery is performed
Cataract surgery is typically performed as an outpatient procedure and takes less than an hour to complete.
The surgery begins with the administration of anesthesia to numb the eye. The two main types of anesthesia used are topical anesthesia, which involves numbing eye drops, and local anesthesia, which involves an injection near the eye to numb it [1]. Many surgeons use a combination of both types.
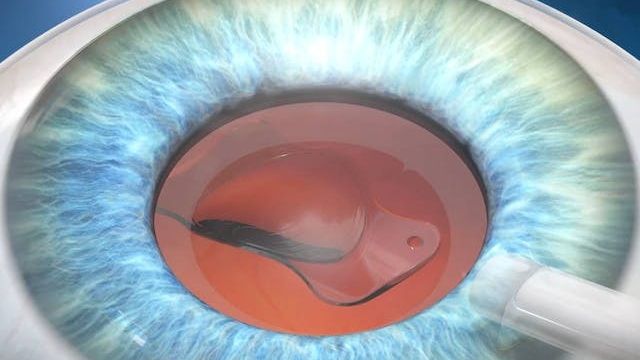
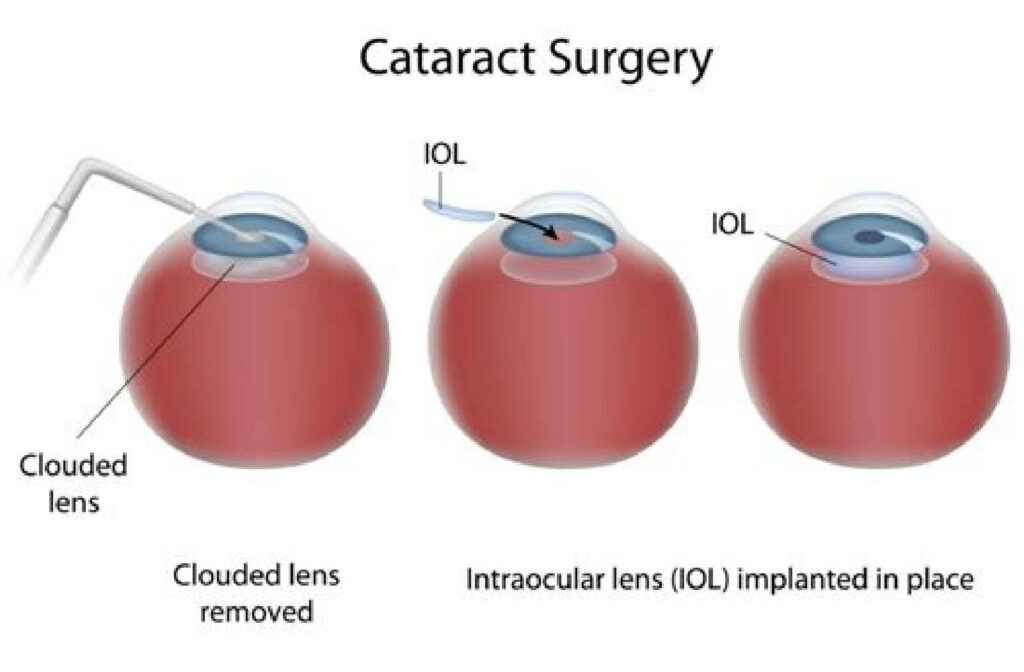
Next, tiny incisions are made in the eye to gain access to the cloudy lens. The clouded natural lens is broken up using an ultrasound probe and suctioned out. Once removed, the natural lens is replaced with a clear artificial intraocular lens (IOL) made of plastic, silicone or acrylic. The IOL is folded and inserted through the tiny incision where it unfolds into place in the empty lens capsule.
After the new artificial lens is in position, the incisions are usually self-sealing requiring no stitches. A protective shield is placed over the operated eye, and the patient is taken to a recovery area. Post-op recovery typically involves wearing an eye shield at night and using medicated eye drops for 4-6 weeks to prevent infection and inflammation. Vision improvement is noticeable within a couple days, though full visual recovery can take several weeks.
Types of intraocular lenses (IOLs)
There are several types of intraocular lenses (IOLs) that may be used during cataract surgery:
Monofocal
Monofocal IOLs focus light at one distance, typically for either near or far vision. They provide crisp vision at the set focal point but require glasses for other distances. Monofocal lenses are the most common type used during cataract surgery according to the American Academy of Ophthalmology (source).
Multifocal
Multifocal IOLs have different zones for near, intermediate, and distance vision. This reduces dependency on glasses by allowing focus at multiple ranges. However, some compromises in quality of vision may occur.
Accommodating
Accommodating IOLs allow the eye to shift focus to different distances by moving backward and forward. They aim to provide a full range of vision but results can vary.
Toric
Toric IOLs correct pre-existing astigmatism in addition to cataracts. By reducing blur and distortion, they can lessen the need for glasses to correct astigmatism.
Determining IOL Type Based on Lifestyle
The type of IOL implanted during cataract surgery should be customized to each patient’s individual lifestyle needs and preferences. According to the American Academy of Ophthalmology (AAO), choosing an IOL involves weighing the pros and cons of different lens types based on factors like occupation, hobbies, and desire for visual independence from glasses or contacts (https://www.aao.org/eye-health/tips-prevention/best-artificial-lens-implant-iol-cataract-surgery).
For example, multifocal IOLs provide near, intermediate, and distance vision by distributing light to multiple focal points. This reduces or eliminates the need for glasses for some activities post-surgery. However, multifocal IOLs may not be ideal for those whose hobbies or jobs require excellent night vision, as they can cause glare or halos around lights (https://www.dukehealth.org/blog/choose-right-artificial-lens-your-cataract-surgery).
Toric IOLs specifically correct pre-existing astigmatism and can reduce dependence on glasses for those with this condition. However, toric IOLs don’t help with presbyopia, so reading glasses may still be needed after surgery.
Having an in-depth discussion with your ophthalmologist about your lifestyle and visual needs can help determine if a multifocal, monofocal, or toric lens will provide you with the best possible outcome after cataract surgery.
Will glasses still be needed after surgery?
For many cataract surgery patients, some dependence on glasses may remain after surgery, especially for tasks like reading or computer use (Dr Simon Skalicky, 2022). However, cataract removal can substantially reduce but not completely eliminate the need for glasses (Moscow Family Eye, 2023).
The reason is that while cataract surgery can restore clear vision by replacing the cloudy natural lens, other pre-existing refractive errors may remain. These include nearsightedness, farsightedness, astigmatism, or presbyopia (the age-related loss of near vision focusing ability) (Center for Sight, 2022).
Therefore, patients considering cataract surgery should not expect perfect vision without any glasses afterwards, but the surgery can significantly improve vision and reliance on glasses in most patients (Skalicky, 2022). Discussing specific lifestyle needs and goals with your ophthalmologist can help determine the likelihood of reduced glasses dependence after cataract surgery.
When vision changes after cataract surgery
It’s common for some vision changes to occur in the months after cataract surgery as the eyes continue healing and adjusting. Two main causes of vision changes post-surgery are post-operative refractive errors and the development of age-related presbyopia.

Refractive errors like nearsightedness, farsightedness, and astigmatism are caused by the cornea and lens not bending light properly onto the retina. The IOL implanted during cataract surgery aims to correct refractive error, but in some cases the correction is not perfect, leading to residual refractive error. This typically causes blurry vision either for near or distance and may require wearing glasses for certain tasks post-surgery.
Presbyopia refers to the gradual loss of near focusing ability that occurs with aging. As the lens hardens, it becomes difficult for the eyes to zoom in on close objects. Since the implanted IOL cannot adjust its shape like the natural crystalline lens, reading vision is often still required after cataract surgery even with excellent distance vision. This can mean needing glasses for tasks like reading small text.
If vision changes seem to worsen or new symptoms arise months after surgery, it’s important to follow up promptly with your ophthalmologist to determine the cause and discuss options like IOL exchange surgery or prescription eyeglasses to fine-tune vision.
Options for managing residual vision problems
Even with advanced intraocular lenses, some patients may still experience residual refractive errors or vision problems after cataract surgery. There are several options for managing these residual vision issues:
Glasses or contacts for residual refractive errors – Glasses or contact lenses can be prescribed to correct residual nearsightedness, farsightedness, or astigmatism. According to this resource, many patients still need glasses for certain tasks after cataract surgery: https://www.voeyedr.com/blog/training-eyes-after-cataract-surgery/
Mono- to multifocal IOL exchange – If a monofocal lens was originally implanted, it may be possible to exchange it for a multifocal IOL to reduce dependency on glasses. This lens exchange surgery can provide a range of focus for near and far vision.
Refractive laser eye surgery – Procedures like LASIK can also treat residual refractive errors after cataract surgery. This article discusses how laser vision correction is an option to reduce glasses dependence: https://www.yalemedicine.org/news/cataract-surgery-options
Consulting with an ophthalmologist about these options can help determine the best solution for managing visual symptoms after cataract surgery, with the goal of optimization vision and reducing reliance on glasses or contacts.
Achieving the best possible visual outcomes
While cataract surgery is highly effective at restoring vision, some patients may still need glasses or contacts after the procedure. Achieving your personal best visual acuity involves setting realistic expectations prior to surgery, diligently following all post-operative care instructions from your surgeon, and being open to additional vision correction options if needed.
During the pre-operative discussion, your ophthalmologist will explain the likely outcomes based on the health of your eye and the type of IOL implanted. While the goal is to reduce dependency on glasses, most patients will still need some vision correction afterwards, especially for reading. It’s important to understand and accept what your probable results will be.
Closely follow your surgeon’s post-op care instructions, including restrictions on activities, using eye drops as directed, and wearing protective eyewear. Attending all follow-up appointments allows your doctor to monitor your progress and intervene if healing is not on track. Proper rest and care in the first weeks after surgery reduce risks of complications.
If you have residual blurriness, glare, or poor night vision after the eye has fully healed, additional vision correction may be recommended. Options include prescription glasses, contact lenses, or secondary surgical procedures. Your ophthalmologist can suggest the most suitable treatments to help you function optimally.
While cataract surgery cannot guarantee perfection, diligently working with your doctor through the process gives you the best chance of finally being glasses-free or minimizing your need for vision correction afterwards.
Cataract surgery in one vs. both eyes
There are two main options for cataract surgery – having each eye done separately, or having both eyes done at the same time. Having surgery on one eye at a time is known as staggered or sequential bilateral cataract surgery. Having both eyes done in a single surgery session is simultaneous bilateral cataract surgery.
The traditional approach has been staggered surgery, allowing time for the first eye to heal before operating on the second eye. Typically there is a delay of 1 week to 1 month between procedures. The potential advantage of this approach is that it poses less risk should a complication occur.
However, research increasingly shows better visual outcomes with simultaneous surgery. Patients experience improved depth perception, contrast sensitivity and reduced risk of falls when both eyes are corrected at once. Vision between the first and second surgeries can cause visual imbalance. With both eyes done together, patients adapt faster to the new lens and have improved functional vision in the critical early post-op period.
According to recent studies, simultaneous surgery does not increase risks or complications when performed by an experienced surgeon. Many patients select same-day bilateral cataract surgery to optimize visual rehabilitation. However, staggered surgery may be preferred by some patients or in certain medical cases. Discussing options with the ophthalmologist allows customizing the approach to the patient’s specific needs.
(Source: Cataract surgery: both eyes on the same day or on separate days?)
Future outlook and new technologies
While cataract surgery has improved immensely over the years, there are still new advancements being made to further enhance vision outcomes after surgery. Some areas of innovation include:
Advanced measurement technologies
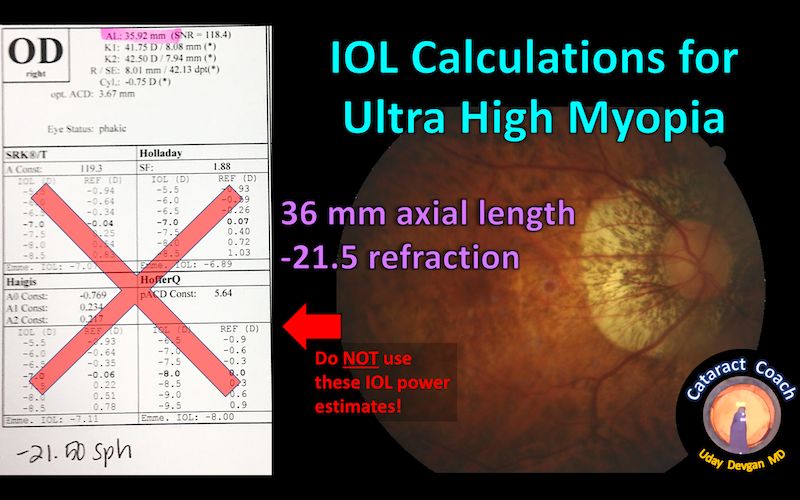
New measurement devices like the Optiwave Refractive Analysis System (ORA) can precisely calculate the optimal lens power needed for each individual eye https://www.yalemedicine.org/news/cataract-surgery-options. This helps reduce the need for glasses or contacts after surgery.
Novel IOL materials and designs
Researchers are developing new types of foldable intraocular lenses (IOLs) using advanced materials like hydrophilic acrylics. These provide high quality optics. Adjustable IOLs are also being perfected, which allow tweaking of the lens power after surgery to achieve better vision https://oomc.com/blog/the-latest-advancement-in-cataract-surgery-light-adjustable-lenses/.
Overall, new technologies are enabling more customized cataract surgery with lenses precisely tailored to the individual. This promises to further improve visual acuity and reduce dependency on glasses or contacts post-surgery.