Cat allergies are caused by an overreaction of the immune system to proteins found in cat dander, saliva or urine. This triggers the release of histamine and other chemicals that lead to allergy symptoms like sneezing, coughing, watery eyes and runny nose. On the other hand, headaches occur when pain-sensitive structures in the head are activated, leading to throbbing pain in the head region. While cat allergies and headaches seem unrelated, there is evidence that allergies can precipitate headaches in some people.
This is because histamine, released during an allergic reaction, causes dilation of blood vessels in the sinuses and surrounding tissues. This swelling of blood vessels can put pressure on pain-sensitive nerves in the head, leading to a headache or migraine. In addition, the immune response during an allergy can cause the release of chemicals called neuropeptides that travel to the brain and contribute to headaches. Therefore, for some allergy sufferers, exposure to triggers like cat dander can initiate an allergic response that ultimately results in a headache.
How Cat Allergies Work
Cat allergies are caused by an immune system response to specific proteins found in cat saliva, skin cells, and urine called allergens. When a person with cat allergies comes into contact with these allergens, their immune system identifies them as foreign invaders and releases antibodies like histamine to attack them. This triggers an allergic response and inflammation. According to The Conscious Parent, cat allergens are extremely lightweight and can stick to clothing and fabric for long periods. Even if the cat is not present, the allergens can circulate in the air and be inhaled, triggering symptoms.
The most common cat allergens are a protein called Fel d 1, which is found in cat saliva and skin, and Fel d 4, which is in cat urine. When cats groom themselves, the saliva dries on their fur and skin and becomes airborne. These microscopic proteins can then be breathed in by people and trigger allergic reactions like sneezing, coughing, and headaches in those with cat allergies. Even harmless activities like a cat rubbing against someone’s leg can transfer allergens to their clothing. Cat dander and fur themselves are not the true culprits of cat allergies. It’s the proteins secreted by cats’ bodies that cause the immune response.

Common Cat Allergy Symptoms
Some of the most common symptoms of cat allergies include:
Runny nose – Allergens like cat dander can cause the release of histamines in the body, which leads to inflammation of the nasal passages and increased mucus production, resulting in a runny nose. This runny nose tends to be clear and thin.
Sneezing – Frequent and sometimes uncontrollable sneezing is another hallmark of cat allergies as the body tries to expel allergens from the nasal cavity. Sneezing attacks may occur in clusters.
Itchy eyes – Cat allergens can irritate the eyes, causing them to become red, watery, and itchy. There may be a scratchy, gritty feeling in the eyes as well. Rubbing the eyes tends to make symptoms worse.
Congestion – Swelling inside the nasal passages caused by an allergic response leads to nasal congestion and blockage. Congestion from cat allergies may cause difficulty breathing through the nose, mouth breathing, snoring, and poor sleep.
How Headaches Occur
Headaches occur due to irritation or compression of key structures in the head and neck. The most important structures involved are the nerves, blood vessels, and tissues surrounding the brain.
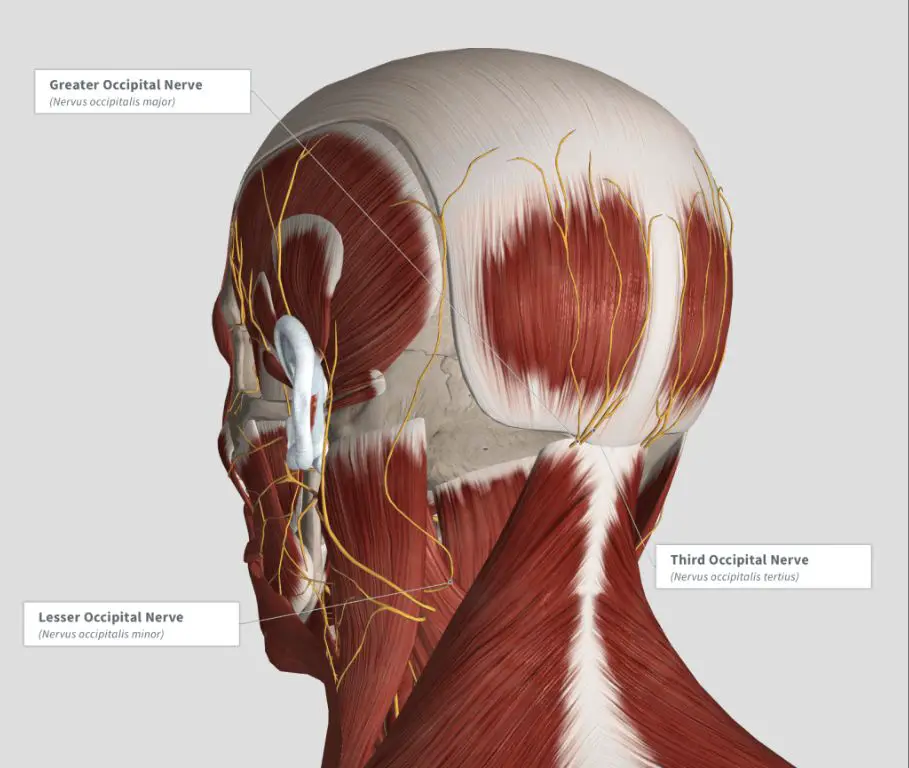
The brain itself does not have pain receptors, but the blood vessels, muscles, nerves and tissues that surround the skull and brain do have pain sensitivity. When these structures are irritated or compressed, they send pain signals to the brainstem and thalamus, which processes pain perception.
Some common sources of headache pain include:
- Dilation or swelling of blood vessels surrounding the brain, which puts pressure on nerves and tissues. This causes vascular headaches like migraines.
- Tension or spasms in neck and scalp muscles, which irritate surrounding nerves. This leads to tension headaches, the most common type.
- Nerve compression or irritation due to neck injuries or structural issues with the spine, skull or tissues. This can result in cervicogenic headaches.
- Changes in brain chemicals or hormones which affect blood vessels and nerves. Hormonal shifts frequently trigger migraine and tension headaches in women.
In many cases, headaches arise from a combination of these factors. Identifying the underlying cause is key for effective treatment and prevention.
The Link Between Allergies and Headaches
Allergies can trigger headaches in a few different ways. One of the most common is through inflammation. When someone is exposed to an allergen, their immune system releases histamine as part of the allergic response. This causes inflammation of the nasal and sinus passages. The swelling and inflammation puts pressure on surrounding nerves which can radiate pain to the forehead, temples, and rest of the head.

Allergies can also cause sinus congestion and blockage which can lead to sinus headaches. As the sinuses get inflamed and swell up, it causes painful pressure and fluid buildup in the sinus cavities located in the face and skull. This added pressure triggers headache pain.
In some cases, allergies may trigger migraine headaches. Researchers believe the chemicals released during an allergic response somehow sensitize the trigeminal nerve which is linked to migraines. The end result is an allergy-induced migraine.
Allergy symptoms like sneezing, itchy eyes, runny nose, and postnasal drip can also strain the head and neck muscles leading to a tension-type headache. Rubbing and blowing the nose repeatedly can tense up those muscles and cause pain.
Overall, there are clear connections between inflammation, sinus pressure, and nerve sensitivity caused by allergies that can directly spur on many different types of headaches including sinus, migraine, and tension headaches.
Prevalence of Allergy Headaches
Studies show that allergy headaches are common, with a significant portion of allergy sufferers also experiencing frequent headaches and migraines. According to research published in a 2013 study, migraine headache was detected in 50% of patients with allergic rhinitis (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3809225/). Another report indicates that 70 to 80% of the North American population experiences headaches, with 15% having headaches weekly or more often (https://www.aaaai.org/tools-for-the-public/conditions-library/allergies/headaches-connected-to-allergies-and-sinus-problem). The data suggests a strong correlation between allergies and headaches in a substantial number of allergy sufferers.
Triggers and Risk Factors
There are several potential triggers and risk factors that can lead to cat allergy headaches:
Exposure to Cats: Frequent exposure to cats is a major trigger for allergy headaches in people with cat allergies. Cat dander, skin flakes, saliva, and urine contain proteins that can provoke an allergic reaction and headache symptoms when inhaled or coming into contact with the skin or eyes. Even short exposures can lead to allergy headache flares in sensitive individuals.
Family History: People with a family history of allergies, asthma, eczema or chronic headaches and migraines are at higher risk of developing allergy-triggered headaches from cat exposure. Genetics play a role in determining immune system responses.
Existing Headaches/Migraines: If someone already suffers from chronic migraines or tension headaches, allergic reactions to cats can exacerbate those existing headache conditions. The inflammation from the allergic response can serve as an additional headache trigger on top of other triggers.
Managing Allergy Headaches
The most effective way to manage allergy headaches is to avoid the triggers that cause allergic reactions in the first place. This may involve keeping windows closed, using high-efficiency air filters, and limiting time outdoors during peak pollen seasons. For pet allergies, restricting the pet from certain rooms and bathing pets regularly can help reduce allergens in the home.
Medications like antihistamines and decongestants can provide allergy relief and reduce inflammation. Antihistamines like loratadine (Claritin) or cetirizine (Zyrtec) block histamine receptors and relieve allergy symptoms. Decongestants such as pseudoephedrine shrink swollen nasal passages. Many combination allergy medications contain both an antihistamine and a decongestant for more complete relief.

Nasal sprays containing corticosteroids like fluticasone (Flonase) or triamcinolone (Nasacort) can reduce inflammation in the nasal passages and sinus cavities. Long-term use of these nasal sprays may help prevent allergy headaches in some people.
For people with severe allergies, immunotherapy in the form of allergy shots can help desensitize the immune system over time. Allergy shots involve being administered increasing doses of allergens over several months. This can significantly reduce allergy symptoms and make allergy headaches less frequent.
While allergy headaches may persist even with treatment, avoiding triggers and using medications can provide significant symptom relief for most people.
Seeking a Medical Diagnosis
If you regularly experience headaches that you suspect may be linked to allergies, it’s important to see a doctor for an evaluation. A physician can help determine if your headaches are truly allergy-related and if so, what specific allergens may be triggering them.
Your doctor will likely ask about your headache symptoms, timing, and potential allergy triggers. They may also perform allergy testing to identify specific IgE antibodies to suspected allergen triggers. Common allergy tests include skin prick testing, blood tests, and patch testing.
Once allergies are confirmed, your doctor can provide advice on avoidance and treatment. They may prescribe allergy medications like antihistamines, nasal sprays, or immunotherapy. For severe allergy headaches, your doctor may refer you to an allergist for specialized testing and treatment.
It’s important to consult a doctor early on rather than self-treating headaches. A physician can rule out other potential headache causes like migraines, identify appropriate treatments, and help prevent unnecessary medication overuse.
Outlook and Prevention
The outlook for allergy headaches is generally positive if the underlying allergies can be properly managed. Avoidance of allergy triggers is key to preventing allergy-related headaches from occurring.
Minimizing exposure to potential allergen sources such as pet dander, pollen, mold, or dust mites can help reduce headache frequency and severity. This may involve using air filters, keeping windows closed at peak allergy times, washing bedding regularly in hot water, and avoiding going outside when pollen counts are high.
Medications can also be an important tool in preventing allergy headache episodes. Antihistamines block the histamine chemical released during allergic reactions, while nasal sprays, eyedrops and other allergy treatments can reduce inflammation. Taking these before exposure to allergens may help stave off headaches.
Allergy shots or immunotherapy represent a more long-term approach to managing the root allergies and minimizing headaches over time. Finding an effective prevention regimen takes some trial and error, but being consistent with avoidance measures and medications as needed offers the best protection according to this source.