What are cataracts?
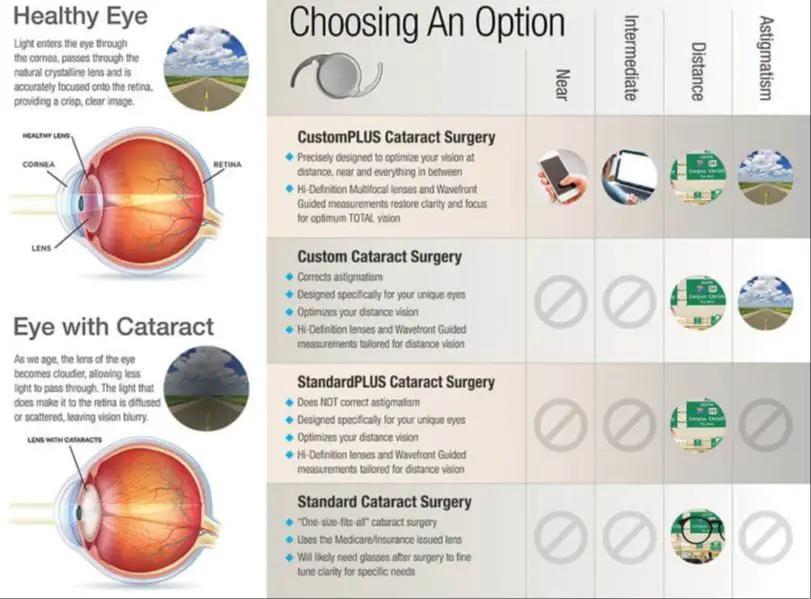
Cataracts are a clouding of the natural lens in the eye that affects vision. The lens is normally clear and allows light to pass through it to focus on the retina at the back of the eye. With cataracts, the lens becomes progressively clouded over time, preventing light from easily passing through and reducing vision (Source).
Cataracts typically form slowly, over many years, as clumps of protein build up in the lens of the eye. These protein deposits scatter light as it passes through the lens, causing blurred or cloudy vision. Eventually the clumps may get large enough to significantly block light from reaching the retina, causing vision loss (Source).
While cataracts can occur in either eye, they usually affect both eyes as a person ages. Over half of all Americans either have a cataract or have had cataract surgery by the age of 80.
Symptoms of cataracts
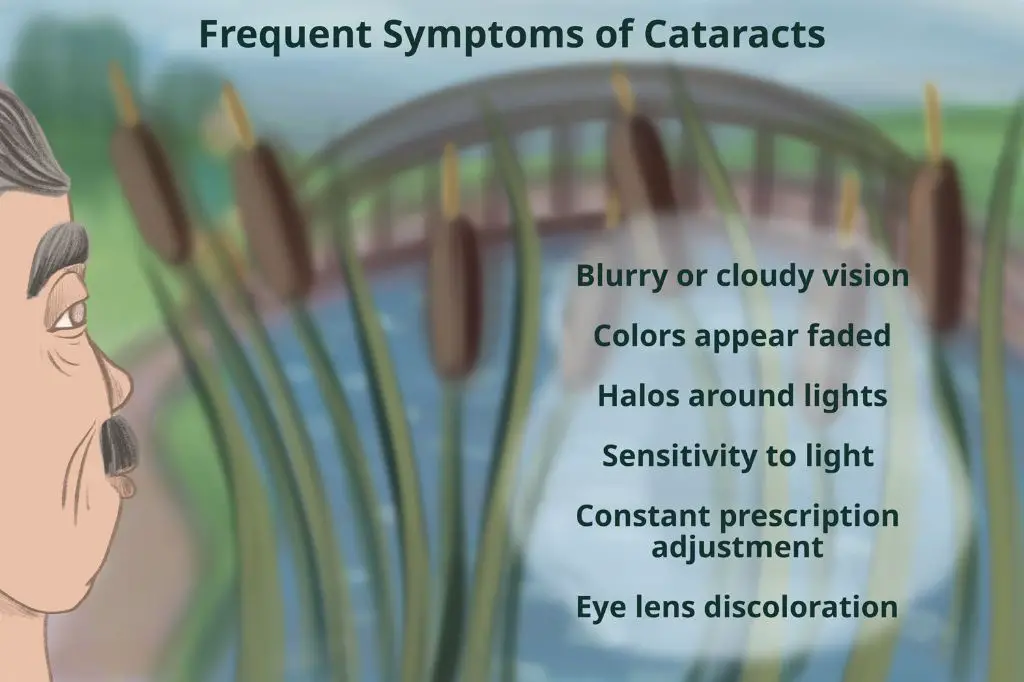
Some common symptoms of cataracts include:
- Blurry vision – With cataracts, your vision may become blurry or cloudy. You may have trouble seeing details or reading small print.
- Sensitivity to light and glare – Catraracts can make your eyes sensitive to bright light. Glare from sunlight or lamps can be bothersome.
- Trouble seeing at night – Cataracts cause difficulty with night vision. You may struggle to see well after dusk.
- Seeing ‘halos’ around lights – You may notice halo-like glows around lights at night.
- Frequent changes in eyeglass prescription – As cataracts worsen, you may need new glasses prescriptions more often.
According to the Mayo Clinic (source), cataracts cause cloudy areas in the lens of your eye leading to vision changes like blurriness and sensitivity to light.
When to consider surgery
Cataracts often don’t require surgery if they aren’t significantly affecting daily life. But cataracts should be removed when they interfere with normal activities and quality of life. Some signs that cataract surgery may be warranted include:
When cataracts make it difficult to carry out daily tasks like reading, watching TV, cooking, or doing household chores, it may be time to consider surgery. As cataracts worsen, they can cause blurry or hazy vision that interferes with normal functioning.
Driving difficulties are a major sign cataracts are severe enough for surgery. Cataracts can make it hard to see street signs, read dashboards, and spot pedestrians or other cars. Driving with impaired vision from cataracts raises safety concerns.
Trouble reading normal print even with glasses, needing much brighter light to see up close, and issues seeing with glare or at night suggest advanced cataracts. Difficulty reading newspapers, books, computer screens, menus, or text messages indicates functional vision loss that may warrant surgery.
The cataract surgery procedure

Cataract surgery involves removing the cloudy natural lens of the eye and replacing it with an artificial intraocular lens implant. The steps in modern cataract surgery are:
1. Anesthesia – The eye is numbed with either topical anesthetic eye drops or local anesthetic injection around the eye. This allows the surgery to be performed while the patient is awake.
2. Tiny incision – The surgeon makes a tiny incision in the cornea to access the cataract-clouded lens. The latest techniques use an ultrasonic probe to break up the lens into small pieces for easy removal.
3. Removal of old lens – The cloudy natural lens is broken up with ultrasound and suctioned out. The lens capsule or “bag” that contained the old lens is usually left intact.
4. Implant new lens – The surgeon folds and inserts an artificial intraocular lens into the empty lens capsule. The incision is so small no stitches are required.
The operation takes around 30 minutes or less. Cataract surgery is usually performed under local anesthesia so patients are awake during the procedure but do not feel any pain.
More info: https://www.mayoclinic.org/tests-procedures/cataract-surgery/about/pac-20384765
Recovery after cataract surgery
Cataract surgery is an outpatient procedure, meaning you can usually go home the same day. Your eye doctor will provide instructions on what to do and what to avoid during your recovery period. Some tips for recovery include:
- Most people can return home the same day as the surgery. You will need someone to drive you home.
- Your eye will be protected with an eye shield or eye covering. Your doctor will advise you on how long to wear this and how to care for your eye.
- You will be given prescription eye drops to promote healing and reduce the risk of infection. It is important to use these drops as directed.
- Your doctor may recommend limiting activities for the first few days following surgery. Avoid strenuous exercise, bending over, heavy lifting, and getting water in your eye.
- Rest your eye when possible by closing your eyes or taking short naps. Do not rub or press on your eye.
- Your doctor will give you a follow-up schedule for additional exams and care after surgery.
With proper post-op care, most people recover fully within a few weeks. However, vision usually improves rapidly within the first day or two after cataract surgery.
Risks and complications
As with any medical procedure, there are risks associated with cataract surgery. While uncommon, the most serious risks include infection, bleeding and swelling.

According to the American Academy of Ophthalmology, the overall risk of serious complications from modern cataract surgery is less than 1%. However, certain complications are still possible.
Infection is one of the most concerning potential complications. Signs of infection include increased eye redness, pain, blurred vision and discharge. According to the Mayo Clinic, the risk of infection is about 1 in 1000. Most infections can be successfully treated with prescription antibiotic eye drops.
Bleeding during or after surgery is another uncommon risk. It is more likely to occur in patients taking blood thinning medications. According to AAO Eyewiki, bleeding usually resolves on its own but may require additional surgery in rare cases.
Swelling and inflammation can occur after surgery. This is usually temporary and can be minimized by taking prescribed anti-inflammatory eye drops. Less than 5% of patients experience persistent swelling.
Retinal detachment, where the retina pulls away from the back of the eye, is a serious complication occurring in about 0.5% of cases. Patients notice new floaters, flashes of light or a curtain over their vision. Urgent treatment is needed to repair the retina.
Alternatives to surgery
While cataract surgery is the only definitive treatment to remove cataracts, some alternatives can help manage symptoms for mild cataracts. These options include:
Stronger eyeglasses – Getting new prescription eyeglasses with anti-reflective coating can sharpen vision by bending light rays properly into the eye. Stronger lenses and magnification can optimize remaining vision. However, glasses cannot reverse cataracts.1
Magnifying lenses – Magnifying glasses, handheld or mounted on spectacles, create an enlarged image, allowing people with cataracts to see text and images with improved clarity and sharpness. These magnifying aids can temporarily improve visual deficits from cataracts.
Improved lighting – Increasing ambient lighting, using lamps, or getting brighter bulbs can all enhance the available light entering the eye. This additional light enables people with cataracts to see better, especially when reading or doing detailed work. Improved lighting aims to counteract the clouded, dimmed vision caused by cataracts.
Costs of cataract surgery
The cost of cataract surgery can vary depending on factors like the type of procedure, additional tests or imaging needed, location and surgeon fees. However, most people in the United States have cataract surgery covered by Medicare or private medical insurance.
According to Medicare claims data, the average cost of cataract surgery ranges from about $1,600 to $2,600 per eye (source). This includes the surgical fees, facility fees and anesthesia. With insurance, out-of-pocket costs are often limited to co-payments of around $100 to $300.
Additional costs beyond the procedure itself can include:
- Pre-surgery eye exams – $100 to $200
- Eye drops after surgery – $50 to $100
- Corrective lenses or upgrades like toric, multifocal or accommodating IOLs – $200 to $3000 per eye
It’s important to check with your eye doctor and insurance provider to get an accurate estimate of the total costs with your specific health plan and eye health profile.
Deciding when to have surgery
When deciding the optimal timing for cataract surgery, it’s important to consult with your eye doctor. They can examine the progression of the cataract and determine if it is negatively impacting vision. According to the Mayo Clinic, cataracts should be removed when they interfere with daily activities and quality of life. But surgery can often be delayed for months to years in many cases.
There are some lifestyle factors to consider as well when scheduling cataract surgery. Those who are still actively working may wish to have surgery sooner so vision impairment does not affect their job performance. People who are retired may be able to delay surgery longer. Driving at night, reading, computer use, and watching TV are common activities impacted by cataracts that may influence timing of surgery.
It’s advisable to monitor cataract progression at regular eye exams. Your ophthalmologist can help determine when surgery is recommended based on exam findings and symptoms. Delaying too long can increase surgical risks and make implanting an artificial lens more difficult according to Dr. Simon Skalicky. But for most, it is safe to wait for surgery until functional vision loss warrants cataract removal.
Conclusion
When deciding when to have cataract surgery, there are a few key considerations to keep in mind:
- How much your vision is impacting your daily life and activities
- Your eye doctor’s recommendations based on the progression of your cataracts
- Your general health and ability to have surgery safely
- Your lifestyle and visual needs
- The costs involved and your insurance coverage
- Your alternatives if you delay surgery, like new eyeglasses, anti-glare lenses, magnifying lenses, or brighter lighting
While it’s possible to wait up to a year for cataract surgery in many cases, the decision depends on many individual factors. Some people may choose to have surgery sooner if their cataracts are progressing quickly and impacting their daily activities. Others may tolerate mild vision changes for longer before opting for surgery.
Ultimately, the ideal timing is unique for each person. It’s important to have open discussions with your eye doctor to determine when cataract surgery is truly needed for your circumstances and vision goals.