Cat bites are puncture wounds caused by a cat’s teeth. Though small, cat bite wounds can lead to potentially serious infections that require medical treatment. Cat bites have a high risk of infection compared to other animal bites because of the bacteria in a cat’s mouth. Understanding the risks, signs of infection, and proper care can help prevent complications from a cat bite.

Signs of Infection
Cat bites can often cause infections because their sharp teeth can puncture deep into the skin, depositing bacteria deep in the wound. According to the CDC, some signs of infection from a cat bite include:
Redness and swelling around the bite wound – This indicates inflammation and can be a sign of infection setting in. As the CDC notes, “Redness, swelling, draining pus, or pain at the bite wound” are common symptoms.
Pus draining from the bite – Draining pus is a telltale sign of infection, as white blood cells rush to the area to fight bacteria.
Pain around the bite – The bite area may become increasingly painful as infection develops, due to inflammation and irritation.
Fever – An elevated fever can indicate that the body is fighting an infection from the cat bite. Fevers are a key immune response.
According to an article on WebMD, pain, redness and swelling around the bite, along with discharge of pus, are some of the most common signs of infection after a cat bite or scratch [1].
Risk Factors
Certain factors can increase the risk of infection from a cat bite wound. These include:
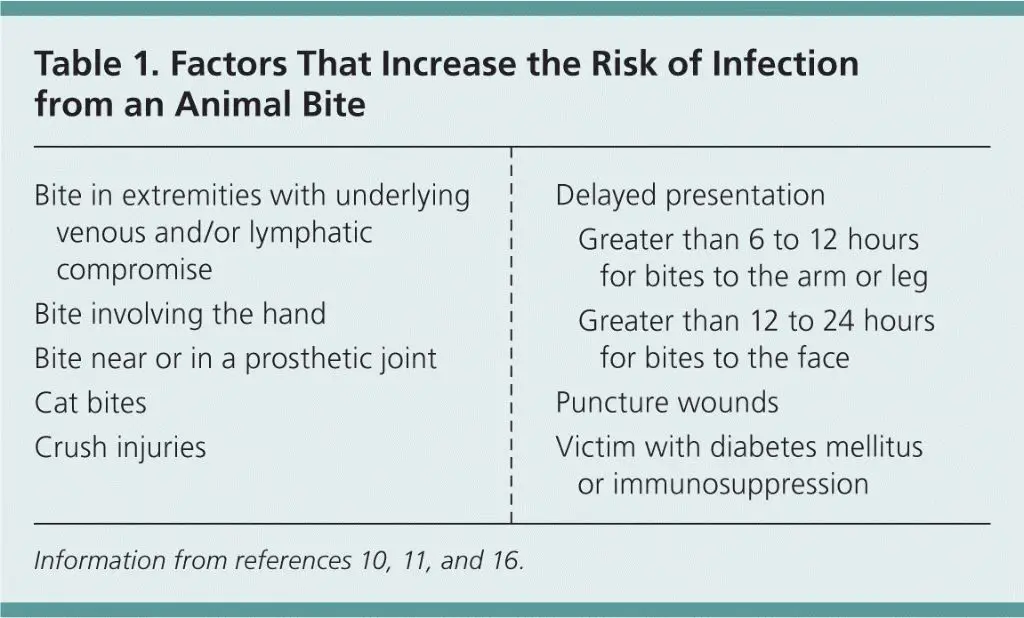
Bite depth – Deeper bite wounds that penetrate deeper into the skin and tissue have a higher risk of infection. Puncture wounds from cat fangs are especially prone to infection. According to a study published in the Annals of Emergency Medicine, 56% of cat bites were puncture wounds [1].
Cat’s teeth – A cat’s teeth are sharp and thin, allowing deep penetration into tissues. Their teeth also harbor bacteria that can enter the wound [2].
Location of bite – Bites to the hand have a higher infection risk as the many joints and small bones allow bacteria to spread more easily into tissues. Bites on the face and genitals also have high infection risk [1].
Health conditions – People with weakened immune systems, diabetes, cancer, or taking medications like steroids or chemotherapy have a higher risk of infection and complications [3].
Types of Infections
The most common bacteria found in infected cat bite wounds is Pasteurella multocida, occurring in over 50% of infections according to one study (Abrahamian, 2011). Pasteurella bacteria are normal flora in the mouths of many animals, including cats and dogs. The bacteria can cause rapidly progressing soft tissue infection and bone/joint infections after an animal bite.
Other common bacteria include streptococcal species such as Streptococcus pyogenes, Staphylococcus species, and anaerobic bacteria like Fusobacterium, Bacteroides, Prevotella, and Porphyromonas (Nocera, 2014). Anaerobic bacteria thrive in the low oxygen environment under the skin’s surface. These bacteria can lead to abscess formation if not treated promptly with proper antibiotics.
When Antibiotics Are Needed

Antibiotics are often prescribed for cat bites that break the skin. Moderate to severe bites, especially deep puncture wounds, have a high risk of infection and often require antibiotics [1]. People with weakened immune systems, such as the elderly, diabetics, or those on immunosuppressant medications, should also receive antibiotics as a precaution [2].
Signs of an infected cat bite wound include increasing pain, swelling, redness, warmth, and pus or foul-smelling drainage. Fevers, chills, and streaks of redness extending from the wound are also concerning signs. In these cases, antibiotic treatment is essential to treat the infection [3].
Antibiotic Options
The antibiotic of choice for cat bites is amoxicillin-clavulanate (Augmentin). Amoxicillin-clavulanate covers the most common bacteria found in cat bites, including Pasteurella, Staphylococcus, Streptococcus, and anaerobes [1]. The typical dosage is 40mg/kg/day divided into 3 doses. Amoxicillin-clavulanate is well tolerated with few side effects.
For people allergic to penicillin, doxycycline is often used instead of amoxicillin-clavulanate. Doxycycline covers Pasteurella, Staphylococcus, and some anaerobes. Clindamycin is another option for penicillin-allergic patients. It covers anaerobes but not Pasteurella [2].
Third generation cephalosporins like ceftriaxone can also be used, but they don’t cover anaerobes as well as amoxicillin-clavulanate. Ceftriaxone requires intravenous administration.
Alternative Treatments
In addition to antibiotics, there are some alternative treatments that may help treat a cat bite wound. These include:
Wound Cleaning
Thoroughly cleaning the cat bite wound is essential, as cat bites often become infected. The wound should immediately be washed with mild soap and warm water. Strong pressure should be applied to induce bleeding to help flush out bacteria (Medscape). Sterile saline or tap water can be used to irrigate the wound (PMC). Avoid using antibiotic or iodine solutions, as they may increase the risk of infection.
Tetanus Shot
If it has been more than 5 years since the patient’s last tetanus shot, or if they are uncertain of their vaccination status, a tetanus booster shot is recommended after a cat bite (AAFP).
Pain Medication
Over-the-counter pain relievers like acetaminophen or ibuprofen can help relieve pain and inflammation at the bite site. Topical antibiotics like bacitracin may also help prevent infection.
Home Care
Home care for cat bites focuses on keeping the wound clean to prevent infection. As soon as possible after being bitten, wash the wound thoroughly with soap and warm water. Use an antimicrobial soap if available. Gently clean around the wound to remove dirt, debris, and saliva. After washing, pat the area dry with a clean towel and apply an antibiotic ointment, such as Neosporin. Keeping the wound bandaged will help keep germs out. Change the bandage daily and check for signs of infection. Elevating the injured area can help reduce swelling and throbbing pain. Over-the-counter pain relievers like acetaminophen or ibuprofen can provide relief from discomfort. Using a cold compress on the bite for 10-15 minutes a few times a day may also help with swelling and pain.
Prevention
You can help prevent cat bites and scratches by being mindful of cat behavior and avoiding actions that may trigger aggression. Here are some tips:
- Avoid startling cats – Move slowly around cats and speak softly to help avoid surprising them. Startled cats may react defensively by biting or scratching.
- Proper pet handling – Pet cats gently, especially on the head and neck area. Avoid petting near the tail and hindquarters which can overstimulate them. Pay attention to a cat’s body language for signs of annoyance or aggression.
- Avoid declawing – Declawing increases biting risk by removing a cat’s primary defense mechanism. Declawed cats are more likely to bite when feeling threatened or play gets too rough. Declawing also poses other risks like infection and chronic pain. Consider alternative deterrents like regular nail trims or soft plastic caps on claws.
With gentle handling techniques and understanding cat behavior, you can reduce the risk of surprise scratches or bites. It’s important to meet a cat’s needs for affection while respecting their boundaries.
When to See a Doctor
You should see a doctor for any cat bite that breaks the skin, as they carry a high risk of infection. According to the VCA Animal Hospitals, cat bites often cause small, deep puncture wounds that can drive bacteria deep into the skin and tissue [1]. Left untreated, a cat bite infection can develop within just 24 hours.

See a doctor right away if you experience any signs of infection, such as [2]:
- Fever or chills
- Increasing pain, swelling, warmth, or redness around the bite
- Red streaks leading from the bite
- Pus or foul-smelling discharge from the bite
- Swollen lymph nodes near the bite
You are also at high risk of infection if [3]:
- The bite is deep or punctured the skin
- You have a weakened immune system
- You have diabetes, cancer, or take immunosuppressant medications
- The bite occurred on your hand, foot, or near a joint
Seeing a doctor quickly can help prevent the infection from becoming serious. Let them examine the wound and determine if antibiotics are needed.