What is Toxoplasmosis?
Toxoplasmosis is an infection caused by the parasite Toxoplasma gondii. This parasite is found worldwide and can infect most warm-blooded animals, including humans (Mayo Clinic, 2022).
People can become infected with toxoplasmosis through various means:
- Eating undercooked, contaminated meat
- Consuming food or drink contaminated with feces from infected animals
- Accidentally swallowing the parasite through contact with contaminated cat litterboxes
- Transmission from mother to unborn baby during pregnancy
Once infected, the parasite spreads throughout the body and remains in tissue cysts, often in the brain and muscles. In most healthy people, the infection produces no symptoms. However, those with weakened immune systems may experience flu-like symptoms, swollen lymph nodes, fever, fatigue, and muscle aches (CDC, 2022).
In rare cases, toxoplasmosis infection can cause damage to the eyes or brain. Infants born with congenital toxoplasmosis may have vision loss, hearing loss, seizures, developmental delays, or mental disability later in life (Mayo Clinic, 2022).
How Humans Contract Toxoplasmosis
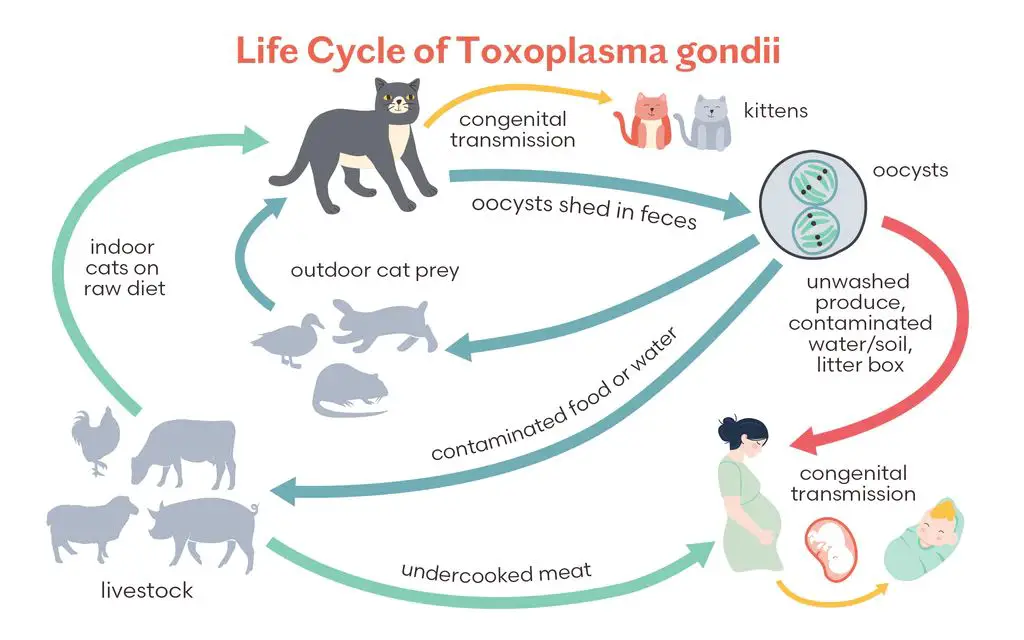
Toxoplasmosis is caused by a microscopic parasite called Toxoplasma gondii. Humans can contract toxoplasmosis in several ways:
Eating undercooked meat: Toxoplasma gondii can be found in undercooked pork, lamb, venison, or beef. Consuming meat that is not thoroughly cooked allows the parasite to survive and infect the body.
Contaminated food or water: The Toxoplasma parasite can contaminate fruits, vegetables, or water sources. Eating or drinking contaminated food and water can lead to toxoplasmosis infection. Proper food handling hygiene and washing fruits/vegetables can reduce this risk.
Mother to fetus transmission: If a pregnant woman becomes infected with toxoplasmosis, she can pass the infection to her unborn fetus through the placenta. This congenital toxoplasmosis can cause serious health complications in the newborn baby.
In summary, the three main ways humans contract toxoplasmosis are by eating undercooked infected meat, consuming contaminated food/water, and a mother transmitting the parasite to her fetus during pregnancy. Proper cooking of meat and washing of fruits and vegetables can help prevent infection.
https://www.cdc.gov/parasites/toxoplasmosis/gen_info/faqs.html
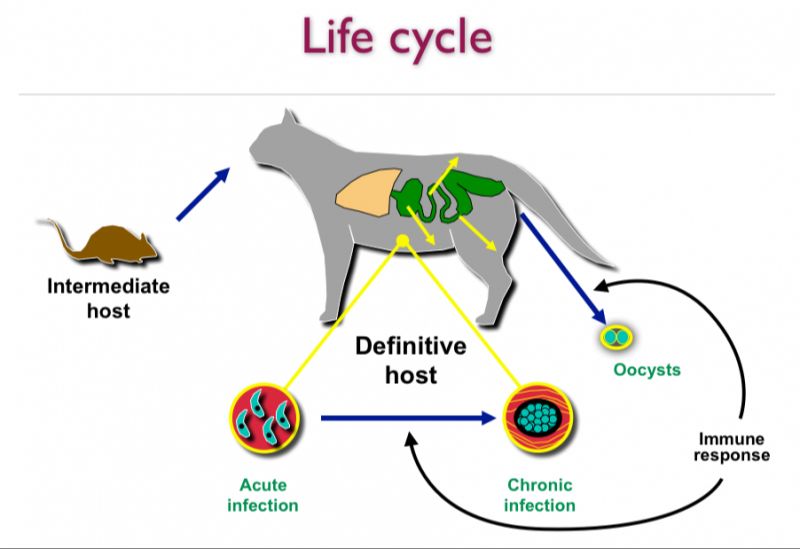
Toxoplasmosis in Cats
Cats get infected with toxoplasmosis by ingesting infected prey, such as rodents, birds, or other small animals. The parasite then forms cysts in the cat’s muscles and brain. Cats shed Toxoplasma parasites in their feces for 1-3 weeks after ingesting the infecting organism. During this time, the feces are infective. However, cats rarely show symptoms when infected. According to VCA Animal Hospitals, an infected cat usually remains asymptomatic because its immune system keeps the parasite from causing illness.
If a cat does develop symptoms, they may include: fever, loss of appetite, lethargy, breathing difficulties, eye inflammation, uncoordinated walking, and seizures. Kittens and cats with weakened immune systems are more susceptible to clinical disease. Pregnant cats can transmit the infection to their fetuses, potentially leading to miscarriage, stillbirth, or kitten mortality. Overall, toxoplasmosis rarely causes significant illness in healthy cats.
Transmission from Cats to Humans
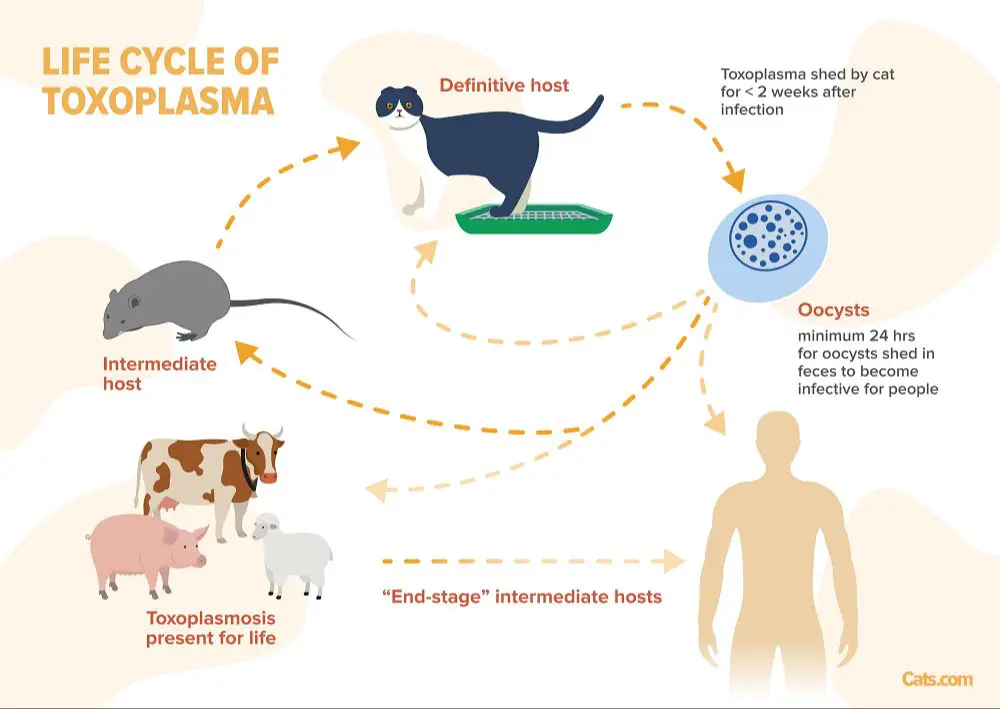
Cats are the main source of human toxoplasmosis infection. The primary route of transmission is through cat feces that contain Toxoplasma gondii oocysts. This usually happens when cat owners clean the litter box and come in contact with cat feces, or touch anything in the environment that has been contaminated with feces (CDC, 2017).
When a cat is first infected with T. gondii, it can shed millions of oocysts in its feces for 1-3 weeks. Even a single cat can potentially contaminate an entire neighborhood or environment. Oocysts can survive in cat feces or soil for over a year and are resistant to many disinfectants and cleaning products. Therefore, any exposure to cat feces, litter boxes, or environments cats have defecated in can potentially lead to toxoplasmosis infection in humans (CDC, 2017).
Proper hygiene is extremely important to prevent fecal-oral transmission. Wearing gloves during litter box cleaning and washing hands thoroughly afterwards can greatly reduce the risk of toxoplasmosis. It’s also critical that pregnant women or immunocompromised individuals avoid cleaning litter boxes entirely.
What Percentage of Cat Owners Have Toxoplasmosis?
Studies show that cat ownership does not appear to be a major risk factor for toxoplasmosis infection. According to research published in PLOS One, the seroprevalence of toxoplasmosis was similar between cat owners (29.4%) and non-cat owners (27.5%) (https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0053508).
Another study published in Emerging Infectious Diseases found the seroprevalence rate among cat owners (30.4%) was not significantly different from non-cat owners (20.8%) (https://wwwnc.cdc.gov/eid/article/15/12/09-0087_article).
While cat owners do not have a higher infection rate overall, some studies show cat-related factors can influence risk. For example, a Frontiers in Veterinary Science study found women cat owners had a higher seroprevalence of 71.4% compared to 36.9% in men cat owners, possibly due to behaviors like cleaning the litter box (https://www.frontiersin.org/articles/10.3389/fvets.2022.927185/full).
In summary, while cat ownership alone does not appear to significantly increase toxoplasmosis risk, certain cat owner behaviors and demographics may impact infection rates.
Precautions for Cat Owners
There are several precautions cat owners can take to reduce the risk of contracting toxoplasmosis from their cats:
Wear disposable gloves when cleaning out litter boxes and wash hands thoroughly afterwards. Toxoplasma gondii oocysts can be present in cat feces and contaminate the litter. Wearing gloves prevents oocysts from coming into contact with bare hands and reduces the chance of accidental ingestion or transmission through touching the face or mouth (CDC).
Keep cats indoors to prevent them from hunting and ingesting infected rodents or birds. This reduces their risk of contracting and shedding T. gondii in their feces. Cats that stay indoors are much less likely to be sources of infection (CDC).
Have another family member change the litter box if you are pregnant or immunocompromised. Avoid all contact with cat feces to eliminate the risk of exposure to T. gondii oocysts.
Wash hands after touching cats, their toys, bedding, food bowls, etc. Good hygiene helps prevent the accidental ingestion or transmission of oocysts.
Testing for Toxoplasmosis
Toxoplasmosis is diagnosed through blood tests that check for antibodies to the Toxoplasma gondii parasite. There are two types of blood tests available:
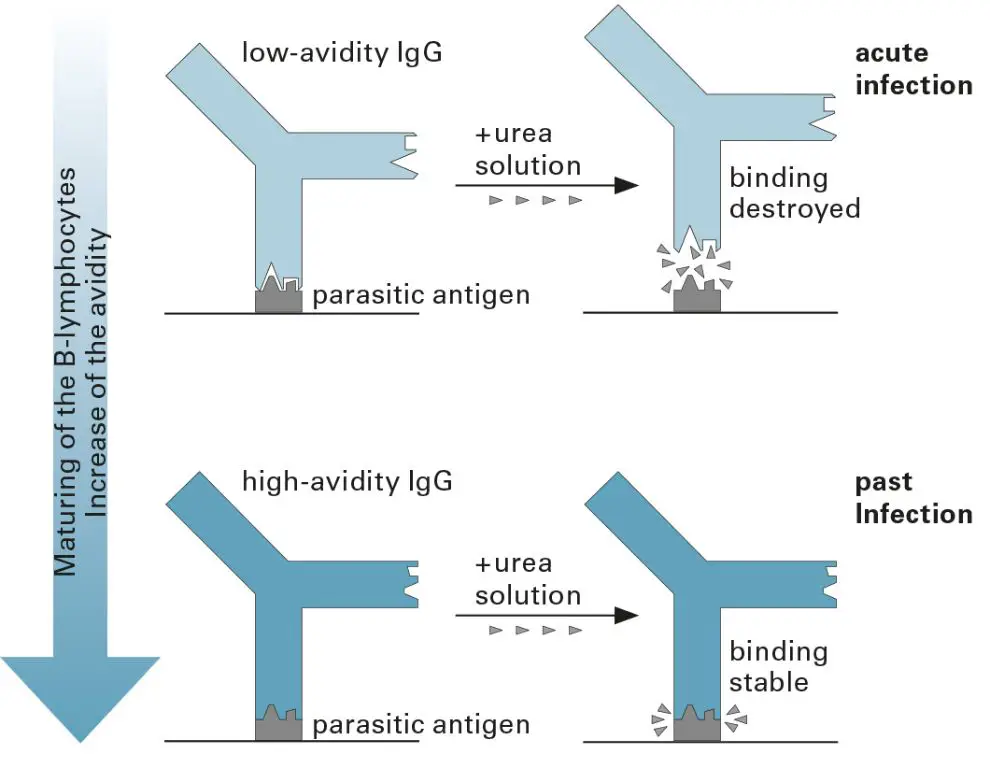
IgM antibody test – This test looks for IgM antibodies, which are the first antibodies the body makes when infected with toxoplasmosis. A positive IgM test means you likely have an active infection.
IgG antibody test – This test looks for IgG antibodies, which the body produces over time as an infection becomes chronic. A positive IgG test means you have been infected with toxoplasmosis at some point in your life but does not distinguish between a recent and past infection (1).
The IgM antibodies only stay in your blood for a few months whereas the IgG antibodies remain for life. Often, both tests are done together to help determine whether the infection is recent or occurred in the distant past (2).
While blood tests for toxoplasmosis are available, they are not routinely performed on asymptomatic individuals such as cat owners. Testing is more commonly done in pregnant women to check for infection and determine potential risks to the fetus.
(1) https://www.cdc.gov/parasites/toxoplasmosis/diagnosis.html
(2) https://www.mayoclinic.org/diseases-conditions/toxoplasmosis/diagnosis-treatment/drc-20356255
Treatment for Toxoplasmosis
Toxoplasmosis is treated with a combination of anti-parasitic medicines and antibiotics to stop the parasite Toxoplasma gondii from spreading in the body. According to the CDC, common medications used include:
- Pyrimethamine – An anti-parasitic medication that interferes with folic acid production in the parasite.
- Sulfadiazine – An antibiotic that stops parasite growth.
- Folinic acid – Helps reduce side effects from pyrimethamine.
Treatment typically lasts for 2-6 months depending on whether the infection is acute or chronic. Pyrimethamine and sulfadiazine work synergistically to eliminate infection in most patients (CDC, https://www.cdc.gov/parasites/toxoplasmosis/health_professionals/index.html).
In some cases, other antibiotics like azithromycin or atovaquone may be used instead of sulfadiazine. Corticosteroids can also help reduce inflammation in severe cases. Treatment aims to quickly eliminate the parasite and prevent long-term complications like eye damage.
Prevention Tips
There are several ways to help prevent contracting toxoplasmosis from cats according to the CDC and Minnesota Department of Health:
Cook all meat thoroughly until it reaches an internal temperature high enough to kill pathogens like Toxoplasma. Use a food thermometer to ensure meat reaches a safe minimum internal temperature, which is 145°F for whole cuts of beef, pork, veal, and lamb, followed by a 3-minute rest time. Ground meats should reach an internal temperature of 160°F.
Wash all fruits and vegetables thoroughly under running water before eating, cutting or cooking. This removes any oocysts that may be on the surface.
Clean litter boxes daily to prevent oocysts from sporulating and becoming infectious. Wear gloves and wash hands thoroughly afterwards.
Avoid drinking unpasteurized milk and untreated water that may be contaminated with oocysts.
These basic hygiene and food safety practices can greatly reduce the risk of contracting toxoplasmosis from infected cats shedding oocysts in their feces. Proper cooking kills the parasite in meat, washing produce removes surface contamination, and cleaning the litter box regularly limits exposure to feline fecal matter containing oocysts.
The Bottom Line
The risk of contracting toxoplasmosis from pet cats is overall quite low, especially for indoor cats that do not hunt prey. According to the CDC, owning and caring for cats who are kept strictly indoors and fed only canned or dried commercial food poses very little risk of toxoplasmosis transmission https://www.cdc.gov/parasites/toxoplasmosis/toxoplasmosis_catowners.html.
Simple hygiene precautions can reduce any small risk even further. This includes washing hands after cleaning the litter box and before meals, wearing gloves while gardening in areas cats may have defecated, and properly cooking meat. General cleanliness around the home and avoiding ingestion of anything that may contain cat feces is also wise.
While additional precautions may be needed for immunocompromised individuals or pregnant women, the risk of toxoplasmosis from indoor pet cats is minimal. Overall, cat owners do not need to live in fear of contracting toxoplasmosis as long as basic hygiene and common sense precautions are followed.