Cataracts are a clouding of the natural lens in the eye that affects vision. As cataracts develop, they cause the lens to become cloudy and opaque, preventing light from easily passing through to the retina at the back of the eye. This results in blurred vision, sensitivity to light and glare, faded colors, and decreased night vision. Cataracts typically develop slowly over time and can eventually lead to significant vision loss if left untreated.
Cataracts are extremely common, especially in older adults. According to the National Eye Institute, more than 50% of Americans have cataracts or have undergone cataract surgery by the age of 80. As the population continues to age, cataracts are becoming an increasingly significant cause of vision impairment and blindness worldwide.
The symptoms of cataracts can have a major impact on daily activities requiring clear vision. Difficulties with reading, driving, computer use, watching television, and recognizing faces can greatly reduce quality of life. Cataract surgery is the only effective treatment to remove the cloudy lens and restore vision clarity. As cataracts progress, surgery is often required to prevent severe vision deterioration.
Overview of Cataract Surgery
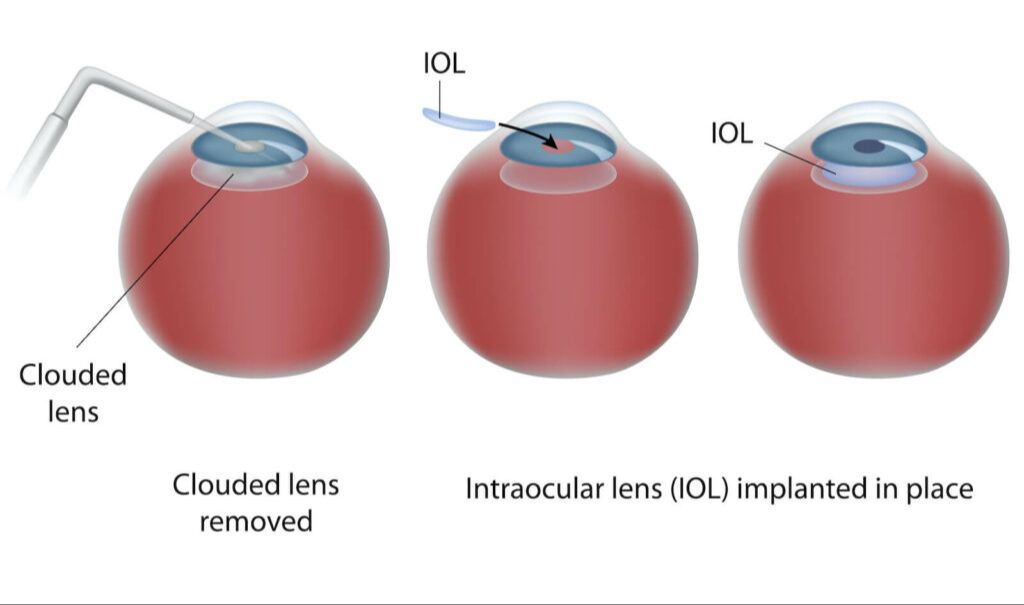
Cataract surgery is a procedure to remove the natural lens of the eye that has developed an opacification, which is referred to as a cataract. The surgery involves making a small incision in the eye to gain access to the lens. The cloudy natural lens is then removed and replaced with an artificial intraocular lens implant.
There are two main techniques used during cataract surgery:1
- Phacoemulsification (phaco) – The standard approach, which uses ultrasound waves to break up the lens before suctioning out the fragments.
- Extracapsular surgery – An older technique that removes the cloudy lens in one piece through a larger incision.
Both procedures take around 15-30 minutes to perform. The phacoemulsification technique is most common today as it requires a smaller incision of about 2-3 mm.
What is 20/20 Vision?
20/20 vision refers to normal visual acuity. Specifically, 20/20 vision means being able to see clearly at 20 feet what someone with normal eyesight should see at that distance. If you have 20/20 vision, you can see an object as sharply and crisply at 20 feet away as a normal eye could see that same object if it were only 20 feet away.1
The 20/20 notation is a common way of expressing visual acuity. The first number refers to the testing distance in feet, while the second number indicates the distance at which a person with normal eyesight could read the same line on an eye chart. So if you have 20/40 vision, it means you can see at 20 feet what a person with normal vision can see at 40 feet. 20/20 is considered normal or optimal eyesight.
Does Cataract Surgery Restore Perfect Vision?
While cataract surgery is highly successful at restoring vision clarity, some people have unrealistic expectations that it will give them perfect 20/20 vision. However, there are many factors that impact the visual outcome after surgery.
According to a study published in the Journal of Cataract & Refractive Surgery, around half of patients achieved 20/20 vision or better after cataract surgery, while 90% achieved 20/40 vision or better. However, several factors affected the likelihood of achieving 20/20 vision, including pre-existing eye conditions like astigmatism and age-related macular degeneration.
The type of artificial lens implant can also impact results. Standard monofocal lenses only correct distance vision, so some patients still need reading glasses afterwards. Premium toric, multifocal or extended depth of focus lenses provide a greater range of vision but can also increase side effects like glare and halos. Individual healing and neuroadaptation to the new lens implant can vary as well.
While great vision gains are achievable with cataract surgery, patients need to understand it does not necessarily guarantee perfect vision. Discussing personalized expectations with your eye doctor based on your eye health profile is important.
Achieving 20/20 Vision After Cataract Surgery
Achieving perfect 20/20 vision after cataract surgery depends on several factors related to eye measurements and surgical precision. The goal is to implant an intraocular lens (IOL) that correctly focuses light on the retina, compensating for any refractive errors like nearsightedness or farsightedness.
Prior to surgery, the ophthalmologist will conduct tests to determine the axial length and corneal curvature of the eye. These measurements help calculate the appropriate power and placement of the IOL. Selecting the optimal IOL for each patient is crucial for optimizing post-surgery vision. Newer formulas and technologies have improved IOL calculations.
During surgery, precision is needed when creating the capsulorhexis opening and implanting the IOL in the exact planned position. Any deviation can result in refractive surprises. Recent advances like femtosecond lasers, intraoperative aberrometry, and O.R. integrated biometry can improve surgical precision.
While these steps help maximize the chances of 20/20 vision, it is not guaranteed. Factors like pre-existing astigmatism, higher order aberrations, capsule opacification, and more can still impact vision quality, even after flawless measurements and surgery. Additional fine-tuning procedures may be needed after cataract surgery to further improve vision.
For more details, see: https://www.londonvisionclinic.com/can-cataract-surgery-give-you-20-20-vision/
Other Factors Affecting Post-Surgery Vision
While cataract surgery can significantly improve vision, there are other factors that can impact the sharpness and clarity of vision after the procedure. Common eye conditions that may lessen the level of vision improvement include:
Astigmatism – An imperfection in the cornea that causes blurry vision. Astigmatism is very common, and often worsens after cataract surgery. Additional treatment such as specialized eyeglasses, contact lenses or laser surgery may be needed to correct astigmatism after cataract surgery.
Glaucoma – Increased pressure inside the eye that damages the optic nerve. Glaucoma cannot be cured by cataract surgery. Ongoing treatment to control eye pressure will be needed after surgery to protect vision.
Age-related macular degeneration – Damage to the retina’s macula. AMD causes loss of central vision and detail, and worsens over time. Cataract surgery does not cure or improve macular degeneration.
Diabetic retinopathy – Retinal damage caused by diabetes. Uncontrolled blood sugar levels can cause new blood vessels to form and bleed into the vitreous humor, obscuring vision. Good diabetes management is key before and after cataract surgery.
If other eye diseases are present, cataract surgery may only partially improve vision. Proper management of any comorbid eye conditions is crucial for optimizing visual acuity after cataract removal. Discuss any other vision or eye health concerns with your ophthalmologist when considering cataract surgery.
Vision Rehabilitation After Cataract Surgery
Vision rehabilitation and follow-up care are important parts of the recovery process after cataract surgery. While the surgery replaces the cloudy natural lens with a clear artificial lens, some patients may still need glasses or contacts after surgery to help optimize their vision.
Many patients are able to see quite well after surgery, especially those that had advanced cataracts before the procedure. However, some may experience refractive errors like nearsightedness, farsightedness or astigmatism that require corrective lenses. The ophthalmologist will prescribe eyeglasses a few weeks after surgery to help correct any residual refractive error and further refine vision.
For those hoping to be less dependent on glasses, advanced technology intraocular lenses like multifocal or accommodating IOLs may be an option. As discussed in this study, multifocal IOLs can effectively restore vision at multiple distances, reducing the need for glasses while driving, reading or using the computer.
If glare, halos or other visual side effects persist after surgery, additional minor procedures can refine the visual outcome. An ophthalmologist may recommend laser surgery to smooth irregularities or adjust the lens position to optimize vision recovery.
With the proper postoperative care and vision rehabilitation, most patients experience significantly improved vision and quality of life after cataract surgery.
Cataract Surgery Complications
While cataract surgery is generally very safe and effective, there are potential risks and side effects to be aware of. Some of the more common cataract surgery complications include:
Inflammation – Most patients experience some inflammation after surgery which can cause eye pain, irritation, and light sensitivity. This is usually temporary and can be managed with anti-inflammatory eye drops.[1]
Infection – There is a small risk of developing an eye infection after surgery. Symptoms include increased eye pain, vision changes, and discharge. This requires prompt treatment with antibiotic eye drops or other medication.[2]
Bleeding – Minor bleeding inside the eye during surgery typically resolves on its own. More severe bleeding is rare but can reduce vision if not addressed.[3]
Swelling of the retina – Called cystoid macular edema, this can cause blurred or distorted central vision. It often improves over time and may be treated with medication.[3]
Dislocation of the implanted lens – The artificial lens may become de-centered or dislocated, requiring a second surgery to reposition or replace it. Proper head positioning after surgery reduces this risk.
Posterior capsule opacification – Scar tissue forms behind the implanted lens, causing blurred vision again after surgery. An outpatient laser procedure can treat this complication.
While risks do exist, cataract surgery is quite safe in the hands of an experienced surgeon. Being aware of potential complications allows patients to watch for concerning symptoms and follow their doctor’s post-op care instructions closely.
When to Consider Cataract Surgery

Cataracts tend to develop slowly over many years. In the early stages, stronger glasses, brighter lighting, anti-glare sunglasses, or magnifying lenses can help compensate for vision changes. But once cataracts begin noticeably affecting your vision and daily activities, it’s a good time to consider surgery.
Your ophthalmologist will diagnose cataracts through a comprehensive eye exam. They’ll check your vision with and without glasses, test your peripheral vision, inspect the retina, and examine your eyes with a bright light to look for cloudy areas. If cataracts are present, they’ll determine whether surgery is warranted based on several factors:
- Blurry vision
- Seeing double or multiple images
- Increased sensitivity to light and glare
- Fading or yellowing of colors
- Impaired night vision
Cataract surgery is generally recommended when cataracts limit your daily activities and quality of life. Early surgery can prevent falls and injuries from poor eyesight. Many people get cataract surgery when vision in one eye decreases to 20/50 or worse. But the choice depends on your lifestyle needs and eye exam results. Discuss goals and timing with your ophthalmologist to determine what’s best for your eyes.
Conclusion
In summary, while cataract surgery is often very successful at restoring vision clarity by removing cloudy lenses, achieving perfect 20/20 vision after surgery depends on several factors. The severity of the cataract and overall eye health play important roles. Most patients can achieve 20/40 vision or better after cataract surgery, though additional vision correction may still be needed for optimal sharpness. It’s important to have realistic expectations when considering cataract surgery. While vision is typically significantly improved, factors like astigmatism and presbyopia may mean some vision correction is still required post-surgery for tasks like reading. By understanding the benefits and limitations of cataract surgery, patients can make informed decisions and achieve their visual goals.