A cataract is a clouding of the lens in the eye that affects vision. As cataracts progress, they can cause blurry vision, glare, poor night vision, double vision, and fading colors.
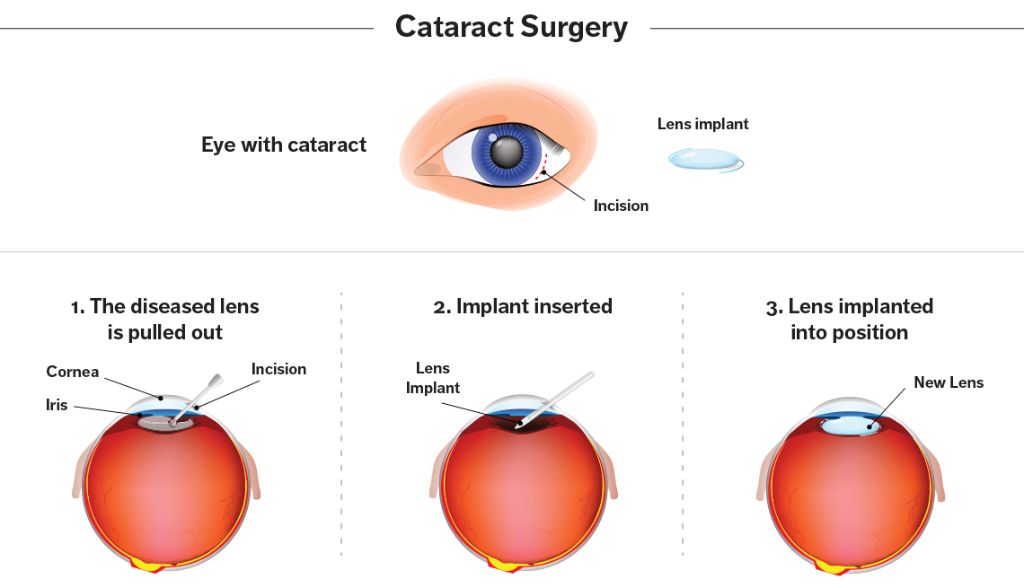
Cataract surgery is a procedure to remove the clouded natural lens and replace it with an artificial lens to restore vision clarity. The standard cataract surgery procedures are phacoemulsification, extracapsular surgery, and intracapsular surgery. Phacoemulsification is the most common and uses ultrasounds waves to break up the cataract into small pieces for removal. Extracapsular surgery makes an incision and removes most of the natural lens while leaving the back lens capsule intact. Intracapsular surgery extracts the entire natural lens and lens capsule in one piece through a large incision.
Evaluating Candidates for Surgery
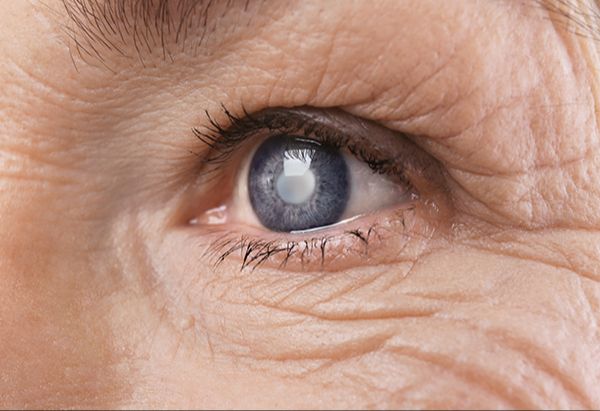
Cataract surgery is typically recommended when the cataracts start to interfere with daily activities like reading, driving, watching TV, and completing work. As the lens becomes cloudier, it can cause blurry vision, sensitivity to light and glare, seeing halos around lights, trouble distinguishing colors, and double vision in one eye. If these symptoms are making it difficult to function normally, cataract surgery may be advised.
According to the Center for Eyecare (https://www.centerforeyecare.net/cataract-surgery/), when cataracts reduce vision so much that normal activities become challenging, it’s time to consider surgery. Surgery is the only effective treatment for cataracts.
Before surgery, the ophthalmologist will do a complete eye exam to evaluate your vision and the severity of the cataracts. They will check your prescription, measure eye pressure, and examine the front and back of the eye. You may undergo tests like optical coherence tomography and corneal topography to get images of the eye. Blood tests may also be ordered to check for any pre-existing conditions like diabetes.
Types of Cataract Surgery
There are three main types of cataract surgery performed today:
Phacoemulsification
This is the most common and preferred method of cataract surgery in the United States. According to HopkinsMedicine.org, over 90% of cataract surgeries are performed using phacoemulsification [1]. In phacoemulsification, the surgeon makes a small incision on the side of the cornea and inserts a probe that emits ultrasound waves to break up the cloudy lens into small pieces. These pieces are then suctioned out. An artificial intraocular lens (IOL) is inserted in place of the natural lens.
Extracapsular Surgery
In extracapsular surgery, the surgeon makes a longer incision on the side of the cornea to remove the cloudy lens in one piece. According to Wills Eye Hospital, this technique requires a larger incision than phacoemulsification [2]. After the natural lens is removed, an IOL is inserted into the empty capsular bag.
Intracapsular Surgery
This is the oldest method and rarely performed today. The entire lens including the surrounding capsular bag is removed through a large incision. According to Focus Clinics, this leaves nothing to support the artificial IOL, so it must be placed in front of the iris [3]. Intracapsular surgery has more complications and requires a longer recovery time than other modern techniques.
Phacoemulsification Procedure
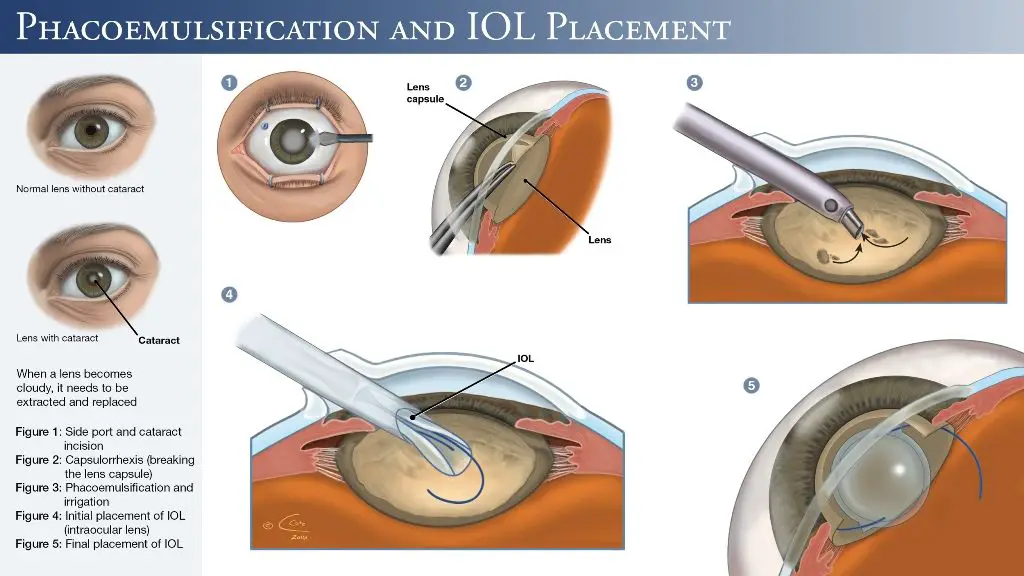
Phacoemulsification is the most common and preferred type of cataract surgery performed today. During phacoemulsification, an ultrasonic probe is inserted through a very small incision in the eye to break up and remove the cloudy lens. Here are the key steps involved in the phacoemulsification procedure:
The eye area is cleaned and numbed with anesthesia. The patient remains awake during the procedure.
The surgeon makes a tiny incision in the cornea, usually less than 3 mm wide.
A viscoelastic solution is injected into the eye to maintain the shape of the eye during surgery.
Using high frequency ultrasound waves, the probe is inserted through the incision to emulsify and break up the cloudy natural lens. The ultrasound waves also aspirate and suction out the fragmented lens pieces.
After the natural lens is removed, the surgeon inserts and secures an artificial intraocular lens (IOL) implant inside the empty lens capsule.
The viscoelastic is suctioned out and the incision is closed, often without any sutures.
A protective shield is placed over the eye at the end of the procedure.
Extracapsular Surgery
Extracapsular cataract extraction involves removing the lens while leaving the back part of the lens capsule intact. The steps include:
Capsulotomy: The surgeon makes an incision in the cornea and creates an opening in the front part of the lens capsule. This allows access to the cataract (Cheap Medicine Shop).
Phacoemulsification: The surgeon breaks up and vacuums out the cloudy lens material through the capsulotomy opening using a special ultrasound device. The back part of the capsule remains (Jaypee Digital).
IOL Implantation: Once the natural lens is removed, the surgeon inserts and secures an artificial intraocular lens (IOL) inside the remaining back part of the capsule.
Intracapsular Surgery
Intracapsular cataract surgery involves removing the entire natural lens and lens capsule in one piece through a large incision. According to Medigac, the steps involve making a 180-200 degree limbal based conjunctival flap, followed by a 11-12 mm corneoscleral incision. The incision goes across the cornea and into the sclera. Then, using cryoextraction, the entire lens including the capsule and zonules are removed in one piece.
Since the entire lens is removed, an intraocular lens (IOL) needs to be placed in the empty capsular bag. The IOL is usually fixated to the iris or sclera with sutures. Because there is no capsular bag for support, the IOL can be less stable and more prone to displacement compared to other techniques where the posterior capsule remains intact.
Intracapsular cataract surgery can fully remove a mature or hypermature cataract through a wide incision, but often results in more post-operative inflammation and a longer recovery time. It also removes the eye’s ability to accommodate or adjust focus, requiring a monofocal IOL for distance vision. This technique has largely been replaced by small-incision phacoemulsification as the standard of care.
Length of Surgery
The length of cataract surgery can vary depending on the specific procedure used as well as other factors.
For routine cataract removal and lens implantation, the surgery typically takes between 10-20 minutes per eye. The most common and fastest method is phacoemulsification, which uses ultrasound waves to break up the cloudy lens and remove it through a small incision. This generally takes 10-15 minutes.
More complex procedures like extracapsular surgery, where a larger part of the lens is removed intact, can take 20 minutes or longer. Intracapsular surgery, which removes the entire lens and capsule, takes the longest at 30 minutes or more per eye.
Factors that can increase the length of surgery include:
- Dense or mature cataracts, which are harder to break up and remove
- Weak zonules, which support the lens
- Small pupil size that needs to be dilated
- Other eye issues like glaucoma or retinal problems
- Patient movement or difficulty cooperating
So while routine cataract surgery is relatively quick, complex cases with complicating factors can lengthen the procedure. But in general, most cataract operations are completed within 10-20 minutes per eye.
Anesthesia
Cataract surgery is typically performed under local anesthesia to numb the eye. This avoids the risks associated with general anesthesia. There are a few options for providing anesthesia:
– Topical anesthesia – Eye drops like lidocaine or tetracaine are applied to numb the surface of the eye. This is often combined with an intracameral injection inside the eye.
– Retrobulbar block – The anesthetic is injected behind the eye to numb the muscles and optic nerve. This provides deeper anesthesia but takes longer to wear off after surgery.
– Peribulbar block – The anesthetic is injected around the eye instead of behind it. This has a lower risk profile than the retrobulbar block.
– Sub-Tenon’s block – The anesthetic is injected in the tissue behind the eye using a small cannula. This targets anesthesia to the muscles around the eye.
– Intracameral injection – The anesthetic is injected into the front chamber of the eye. This provides rapid, short acting anesthesia.
Many cataract surgeries use a combination of topical and intracameral anesthesia to maximize patient comfort while minimizing risks. Sedation medication can also be given intravenously to help patients relax during the procedure.
Recovery Time
The typical healing timeline after cataract surgery is as follows:
- Immediately after surgery – Your vision will be blurry. You’ll need to wear an eye shield to protect your eye.
- 1 day after surgery – Vision should start improving, but will still be blurry. You can remove the eye shield.
- 1 week after surgery – Vision should continue improving. You’ll see your doctor for a follow-up exam.
- 1-2 months after surgery – Vision should stabilize, and you may get a final prescription for eyeglasses.
- 3-6 months after surgery – Any residual blurriness or glare should resolve as the eye fully heals.
Post-op care is critical during the recovery period. Be sure to:
- Use eye drops as directed to prevent infection and reduce inflammation.
- Wear an eye shield at night for at least the first week.
- Avoid rubbing or pressing on the operated eye.
- Wear sunglasses outside to protect from wind and bright light.
- Avoid strenuous activity for 2-4 weeks.
- Use caution around steps or tripping hazards until vision stabilizes.
- Attend all follow-up appointments as recommended by your surgeon.
With proper post-op care, most patients are able to return to their normal routine within 1-2 weeks after cataract surgery. However, maximum vision improvement can take 3-6 months as the eye fully stabilizes.
Conclusion
In summary, the length of cataract surgery can vary greatly depending on the specific procedure, anesthesia needs, and complexity of the patient’s case. However, most routine cataract operations today using phacoemulsification technology take approximately 10-20 minutes of actual surgical time. Patients undergo extensive screening to determine if they are viable candidates for surgery. Selecting appropriate patients and utilizing advanced cataract removal techniques allow ophthalmologists to complete procedures efficiently.
While cataract surgery is generally considered safe and effective, it is still an invasive procedure requiring anesthesia. The pre-op evaluations, surgical preparations, anesthesia administration, and post-op recovery time add several additional hours to the surgery duration. Patients can expect to spend 2-4 hours at the surgical facility. The vast majority of patients experience significantly improved vision following modern cataract surgery. By understanding the general timeframes and procedures involved, patients can have appropriate expectations and recover smoothly.