Introduction to Cataracts
Cataracts are a clouding of the lens in the eye that leads to blurred vision. According to the National Eye Institute, more than 24.4 million Americans over the age of 40 have cataracts.[1] Cataracts are extremely common, especially in older adults, with around 50% of people between the ages of 65 and 74 having some degree of cataracts.[2]
As cataracts develop, they can cause vision problems like cloudy, blurry, or dim vision. Colors may start to look faded, glare from lights may be more bothersome, and vision at night may get worse. Reading and seeing details becomes more difficult. When cataracts progress enough to seriously impact daily activities, cataract surgery is usually recommended to remove the clouded lens and replace it with an artificial lens.
Cataract surgery is indicated when cataracts have matured enough that vision problems interfere with everyday activities like reading, driving, watching TV, and general mobility. Most people who undergo cataract surgery report significant improvement in vision and quality of life.
Evaluating Candidates for Cataract Surgery
Ophthalmologists will conduct a thorough evaluation of a patient’s eyes and medical history before determining if they are a good candidate for cataract surgery. This involves assessing the cataract and its impact on vision, as well as evaluating the health of the eye and body overall.
During the initial consultation, the ophthalmologist will review the patient’s medical history, including any previous eye injuries, surgeries or diseases, and current medications or health conditions. A comprehensive eye exam is performed, which includes:
- Testing visual acuity to determine how well the patient can see at various distances with and without glasses or contacts.
- Measuring intraocular pressure to screen for glaucoma.
- Examining the front of the eye with a slit lamp to look for signs of cataracts or other abnormalities.
- Dilating the pupils to thoroughly evaluate the lens and retina.
Additional specialized tests may be conducted to further assess the cataract and the health of other eye structures. These can include:
- Corneal topography to map the curvature of the cornea and detect irregular astigmatism or other issues (source).
- Ocular coherence tomography (OCT) to examine the retina and measure its thickness.
- Fluorescein angiography to view blood vessels in the retina.
If the cataract is significantly impacting vision and negatively affecting the patient’s quality of life, cataract surgery may be recommended. Good candidates are those with healthy eyes who are reasonably likely to have improved vision after cataract removal. The ophthalmologist will discuss benefits, risks, and alternatives to help determine if surgery is appropriate for that individual.
How Cataract Surgery is Performed

Cataract surgery is typically performed using a procedure called phacoemulsification. This involves using an ultrasound device to break up the cloudy natural lens, then suctioning out the pieces.
The surgery starts with the administration of anesthesia, usually topical and intraocular, to numb the eye. The surgeon then makes a tiny incision in the cornea to access the front of the lens capsule.
Next, the surgeon inserts a thin probe that emits ultrasound waves to break the lens into small fragments. These lens pieces are suctioned out of the eye through the probe. The cloudy lens cortex is also carefully removed.
After the natural lens is removed, the surgeon folds and inserts an artificial intraocular lens implant into the empty lens capsule. The incision is so small that stitches are usually not required.
The operation generally takes less than 30 minutes. Most cataract surgeries are successful, with over 98% of patients reporting improved vision afterwards (https://m.youtube.com/watch?v=ZP6Qqwv3vRo).
Types of Artificial Lenses
There are several types of artificial intraocular lenses (IOLs) that may be implanted during cataract surgery. The most common options include:
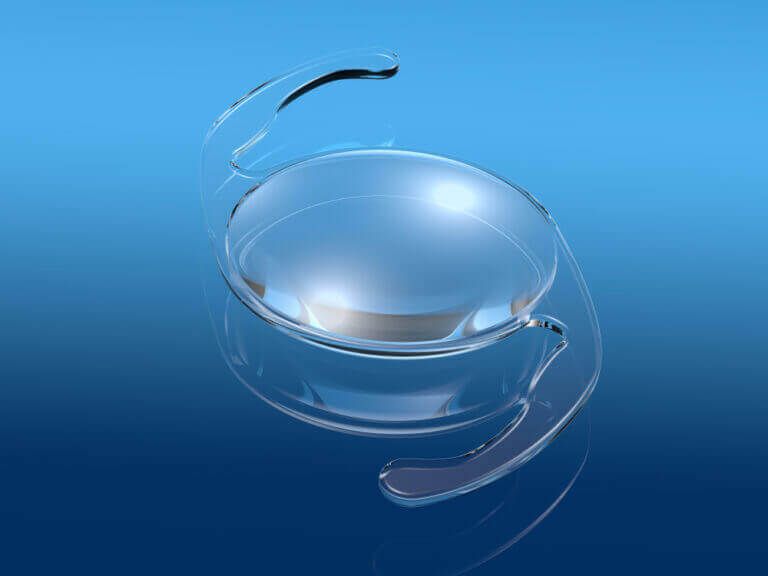
Monofocal IOLs – These provide focus for one distance, usually for far away. This is the most basic type of IOL and the most frequently used. Patients typically still need glasses for reading or computer work. A 2012 study found high satisfaction rates with monofocal IOLs.
Multifocal IOLs – These have different zones for near, intermediate, and far vision allowing reduced dependency on glasses. However, some visual side effects like glare or halos may occur. Multifocal IOLs can provide a fuller range of vision.
Accommodating IOLs – These are designed to shift focus to different distances mimicking the eye’s natural lens. Results can be inconsistent so multifocal IOLs are often preferred.
Toric IOLs – These correct pre-existing astigmatism and improve uncorrected distance vision. They are oriented to the specific axis of the corneal astigmatism.
Recovery Process

Here is what to expect in the recovery process after cataract surgery:
On the day of surgery, you will need someone to drive you home after you are discharged. Your eye will likely have some irritation, swelling, and discomfort. Your surgeon will provide prescription eye drops to aid healing and reduce risk of infection. You will need to wear an eye shield at night to protect your eye as it heals.
Post-surgery restrictions typically include:
- Avoid rubbing or pressing on the operated eye
- No swimming or using hot tubs
- No strenuous activity for 1-2 weeks
- Avoid very bright lights
- No eye makeup for 1-2 weeks
It is crucial to properly administer the prescribed eye drops multiple times per day in the weeks following surgery. This aids the healing process and reduces swelling and risk of infection [1].
Your ophthalmologist will schedule multiple follow-up appointments to monitor your recovery. Vision is expected to improve within the first couple weeks after cataract removal. However, it may take a couple months for your best vision to be realized once swelling has completely subsided.
Potential Surgical Risks and Complications
While cataract surgery is very common and usually successful, there are some potential risks and complications to be aware of. Some of the main surgical risks include:

Infection
There is a small risk of infection developing after surgery. This is estimated to occur in around 0.1% of cases. Signs of infection include increased eye pain, discharge, redness, and vision changes. If an infection does occur, antibiotic eye drops are typically prescribed to treat it (Beach Eye).
Bleeding
Bleeding inside the eye during or after surgery is an uncommon complication. It usually resolves on its own, but may require additional surgery if severe. Using anti-inflammatory eye drops after surgery can help reduce bleeding risk (Zeiss).
Swelling
Inflammation and swelling of eye tissues is common after surgery. This usually resolves within a few weeks with the help of prescription anti-inflammatory eye drops. Severe swelling may temporarily affect vision.
Droopy Eyelid
A droopy eyelid (ptosis) sometimes occurs after cataract surgery if eye muscles or nerves are affected during the procedure. Additional surgery may be required to lift the eyelid if the drooping is significant.
Retinal Detachment
Retinal detachment after cataract surgery is very rare, occurring in around 0.5-1% of patients. Symptoms include sudden flashes of light and “floaters.” If retinal detachment occurs, prompt surgical repair is needed to prevent permanent vision loss (NYEE).
Long-Term Post-Surgery Care
After cataract surgery, ongoing care is important for protecting vision and eye health. Patients should take the following long-term precautions:
Wear sunglasses or protective eyewear when outdoors. Eyes remain sensitive to UV light after surgery, so wearing wraparound sunglasses can prevent damage and irritation (What Side Effects Can You Expect With Cataract Surgery?).
Use prescribed medicated eye drops as directed. These antibiotic and anti-inflammatory drops prevent infection and reduce swelling during the healing process (Can I Still Wear Contacts After Cataract Surgery?). Tapering off drops should be done under an ophthalmologist’s supervision.
Watch for signs of complications. Patients should monitor their vision and check for symptoms like pain, redness, discharge or flashes of light, which could indicate serious conditions like infection, swelling or retinal detachment. Promptly reporting any changes allows early treatment.
Costs of Cataract Surgery
The cost of cataract surgery can vary widely depending on the type of procedure, insurance coverage, and location. However, most people undergoing cataract surgery in the United States will have the majority of the costs covered by Medicare or private medical insurance.
For those with Medicare coverage, out-of-pocket costs typically range from $1,500-$3,000 or more per eye, which includes deductibles and coinsurance payments. Those with private medical insurance can expect to pay anywhere from $1,600-$2,600 per eye, depending on the plan’s coinsurance percentage.
Without any insurance coverage, cataract surgery can cost $6,000-$8,000 or more per eye when paying completely out-of-pocket. However, many ophthalmology practices offer payment plans or discounts for uninsured patients to help make this sight-restoring surgery more affordable.
There are also financial assistance programs available, such as Medicare Savings Programs for those who qualify or non-profit funds that provide eye surgery assistance for low-income, uninsured patients.
Success Rates and Patient Satisfaction
Cataract surgery has a very high success rate. According to studies, over 98% of patients have improved vision after cataract surgery [1]. Many patients report being very satisfied with the results of their procedure. In one survey of cataract surgery patients, 84% ranked their satisfaction as “somewhat satisfied,” “very satisfied,” or “completely satisfied” [2].
Patient testimonials show just how dramatically cataract surgery can improve vision. John S., aged 67, said “I can see clearly again after my cataract surgery. Colors are brighter, street signs are sharper, and I can read books again without straining my eyes.” Sarah R., aged 72, reported “I had trouble seeing at night and struggled to read small print before my surgery. Now my vision is crystal clear at all times of day. I wish I’d gotten this done sooner!”
In studies assessing vision before and after cataract surgery, patients showed significant improvements in visual acuity and contrast sensitivity. After surgery, over 70% of patients achieved 20/40 vision or better, compared to only 4% prior to surgery [3]. Patients also report improvements in doing daily activities like reading, driving, recognizing faces, and watching TV after cataract surgery.
Conclusion
Cataract surgery is a common and generally safe procedure to restore vision loss from cataracts. As covered in this article, the surgery involves removing the clouded natural lens and replacing it with an artificial intraocular lens implant. The operation is done under local anesthesia and takes less than an hour. Most patients experience improved eyesight soon after surgery. While there can be risks of infection and other complications, serious problems are rare when the surgery is performed by an experienced surgeon.
When cataracts begin to interfere with daily activities, surgery is often the best option to regain clear vision. The procedure has high success rates in terms of visual acuity and patient satisfaction. As techniques and lenses continue to advance, cataract surgery may become even safer and more effective in the future. For now, the current methods provide excellent outcomes for most patients with cataracts.
In conclusion, cataract surgery is a well-established procedure that can significantly improve vision and quality of life. When cataracts progression starts impacting a person’s lifestyle and visual acuity, consulting an eye care specialist about surgical options is advisable.